Table of Contents
A guide to Nursing Communication
Meet Steph – The nurse you want next to you when you need help with communication with a patients
Stephanie has a Bachelor of Biomedicine, Bachelor of Nursing from Monash University. She has more than 7 years’ experience working with people with disability and communication issues and this is her passion, having even presented research at ICUR 2017. She is an experienced RN, having worked in many fields but mostly: palliative care, rehab and emergency. She also volunteers as a Registered Nurse and prehospital first responder at music festivals and community events with St John Ambulance.
We chat with AUSLAN Sign Language Educator Gail. Check it out and learn some sign language!
Some other articles you will enjoy
- For a comprehensive and systematic approach to assessment in ICU, read THIS POST
- For a guide to placement/grad year on a cardiac / cardiothoracics ward + free worksheet on cardiac pharmacology and main cardiac issues go HERE
- Cheat-sheet guide for your ICU nursing placement HERE
- Introduction to Cardiac Nursing Basics for nursing students
- The ultimate nursing guide to sepsis
- A cheat-sheet guide for your cardiac nursing placement
- The helpful complete guide to an Aged Care Nursing Placement for students
- 14 strategies for successful clinical placements
- Untangling nursing communication – “My patient can’t talk to me… Help!”
- Step-by-step explanation of nursing CPD
- Helpful list of proven graduate nurse tips!
- You MUST know about ACT-PINCHES (N) drugs
Are they alive?
Okay, so let’s first make sure they’re responding… patent airway… breathing… Still with us and not doing CPR? Great!
There are so many reasons why a patient may have difficulties communicating, be this anywhere from sedation and intubation, to a recent stroke, to even certain disabilities such as cerebral palsy or autism. These will all affect patients in different ways, but hopefully something here will relate to your patient!
Is this normal?
How do I know if this is normal?
This is actually really important to consider. Have a look at your handover sheet and nursing care plan for information on the patient’s communication and history. Hopefully you will have been told during handover about key conditions that may affect a person’s ability to speak!
If you aren’t sure, and can’t find information, run through your DRSABCD. Some conditions such as stroke can cause an expressive or receptive dysphasia (meaning a patient can’t say the right words, or understand your words). If this is unusual for the patient, definitely speak with your nurse in charge and raise the possibility of a MET call. Some conditions can also cause aphasia too – panic attacks and seizures are a possibility. If you aren’t sure – get someone involved. Much better to be safe than sorry!
I suppose as well… sometimes patients are deaf/Deaf. If they aren’t looking at you – they may not know that you’re talking to them. Just something else to rule out! :p
My patient is saying words that don’t make sense
This is normal… but my patient is saying words that don’t make sense. How do I work out what they are saying?
This is most likely due to expressive dysphasia – it’s very common after certain types of strokes, and in certain brain tumours such as glioblastoma (GBM). Sometimes people just have it with no real reason (*me*) – have you ever forgotten the word you want, or done the classic calling your teacher Mum?
Some people have insight into it, some don’t. It’s a bit easier for people that do retain insight – they can often keep trying to get the right word, or rephrase it. It’s often useful to repeat the sentence back to the person, just to check it is correct (because sometimes what sounds like word salad is actually just a bizarre request!). Sometimes, asking the person to spell the key word can help – if nothing else, you can guess relevant things from the letter they say. Context will be crucial here too, so listen to everything they are saying and use that to guide your responses.
My patient can talk, but I can’t understand them
I often try to keep guessing the person’s meaning until we work it out. If I can’t, I’ll offer to get someone else (especially if they know the patient – there might be common requests!). The key thing here is, do not smile and nod if you do not understand. The patient will know this – it’s insulting, like what they are saying is meaningless. You won’t offend them by working to understand them. All else fails, keep asking yes/no questions to narrow it down. This works in pretty much all situations!
This can be due to anything from a really strong accent to neuromuscular conditions affecting speech (eg Deafness, cerebral palsy, etc). Either way!
I’ll usually try and guess at the key parts of their speech. “You want me to put the… lotion?… Is that right?” And then we’ll get that first word out and I’ll work out the next key part. “On your… arm? No… your leg?” It’s clunky but it can work! I also think listening to only the consonants, or only the vowels, can sometimes help as well to narrow down what the word sounds like. Or, asking them to spell it. You can even ask them to write/draw what they’re after too!
If that doesn’t work, I’ll ask lots of yes/no questions, starting really broad and working down. “Is it something that you want?” – “Is it something you want me to do?”/”Something you want me to grab?” – “Is it in the room?” etc. Yes/no questions are a GODSEND, I swear.
Sometimes again, it’s a matter of fetching someone. If they are culturally and linguistically diverse, finding a family member of someone who speaks the same language might be your best bet.
My patient can’t speak words.
How can I work out what they’re trying to tell me?
This is… tricky. This is where I see most nurses either panic or just plain give up. And it’s really sad, because there are so many non-verbal communication methods out there.
First of all – remain calm. It can be frustrating trying to work out meanings in these situations but getting upset about it is only going to make it harder. Also – please try to forget the assumption that just because someone can’t communicate verbally means they can’t communicate at all. Most can – just in a different way. After all, it’s differently-abled, not less!
If I don’t know about how a person communicates, the first thing I do (after introducing myself!) is ask them to show me a YES response. Just a yes response. Sometimes it will take them awhile (especially if we’re moving into the more severe neuromuscular disabilities). Keep an eye on their face! For some reason, the most common YES indication (beside a nod!) is for a person to look upwards or raise their eyebrows (it’s a similar muscular response).
Other common things is for people to attempt to verbalise a yes (listen to the vowel particularly), stick out their tongue, or smile. Some people use buttons at home for yes/no communicating as well, so sometimes they’ll look to one side, or raise one hand. Whatever the response is – the key thing is to identify it. So I’ll make them do it twice (once to see what it is, the second time to make sure it was a deliberate response and not a twitch). When we’ve established their YES, I’ll then get them to show me their NO. This then allows me to use YES/NO questions to their standard communicating ability.
Communication Aids
Some people have communication boards or books. There are lots of different ways of using these, but if you see a family member/carer/friend using one with your patient, definitely ask them to show you how it works! Communication boards are usually easier – it’s one board, sometimes double-sided, and often the person will either point or look at the square they want. This square can be as simple as hurt to as complex as Please make me a thickened coffee with milk and two sugars (yes, I have seen that one before!). Definitely look at your patient when using these, and double-check you’re understanding them correctly.
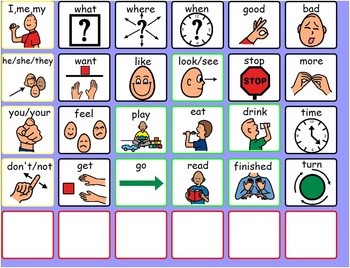
Some patients use technology to communicate. There are heaps of apps on tablets that patients may use (too many for me to touch on!). Some people also use LiteWriters – small electronic typewriters that read out what they have written. They may need some assistance to set these up, if they’ve brought them in to hospital.
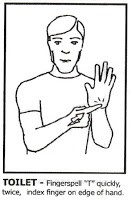
Some people also use Makaton, or Key Word Signs. It’s a simplified version of English with sign language adding to it. Easiest signs would be good or bad (thumbs up or down, like is common in Australia), and toilet (double-signed T).
Also… Keep in mind there are speech pathologists in most hospitals, and they aren’t just for your patient that can’t stop coughing after every meal. You’re well within your right to page them to help you speak with your patient (or teach you about a communication method)!
Can they understand me?
My patient can’t communicate in any way we understand. Can they understand me?
Most of the time… yes. Please don’t ever assume someone is unintelligent because they can’t talk, and don’t talk to them as if they were a child. I made that mistake my first day working in disability – the next day, at the same house, I found out the lady had been married and had also written several books. Some people do enjoy being spoken to in really bright, sing-song voices. Most will think you’re an idiot.
How do I know that they understand me?
Good question! Sometimes… You don’t know. I always look at someone’s face when I talk to them. Usually, people will brighten if they understand what you’re saying. Sometimes it’s as obvious as a smile. Sometimes their eyes lighten a bit and that’s all you get. It takes a LOT of practise to really tell if someone is understanding you or not when they are passive communicators. I can’t always tell myself. But it’s much better to work under the assumption they can understand. If nothing else – at least you’re engaging with them as an adult human being.
None of the above tips are working!
None of the above tips are working with my patient! How do I work out what they want?
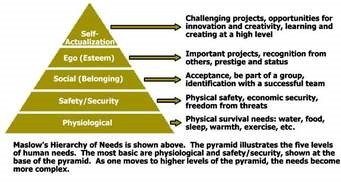
Look at facial expressions and body positioning. If they’re wriggling, they might be uncomfortable. If they’re crying, it might be pain. Offer food and drink, if you can. Check their incontinence aid, if they’re wearing one (also check bony prominences for pressure areas at this point). Look at how they’re positioned in the bed, and use pillows or reposition them if needed. Try analgesia or antiemetics, if they’re written up for some. Sometimes people are just scared too. It’s hard for an able-bodied communicative person to be in hospital, let alone someone with multiple communication and other needs, surrounded by new people who don’t know these things. Sometimes talking to them, or holding their hand, might be all they need. In this case, work through Maslow’s hierarchy of needs until you find the right thing. It might be lots of trial and error, but it’s so rewarding when you do finally work out which need they were trying to communicate J
TL:DR Version
OMG you wrote an entire essay. Can I have the TL:DR version please?
Of course! Here we go:
- Safety first! DRSABCD every time
- Always assume your patient is intelligent – don’t speak to them like a child
- Utilise your resources – family, carers, previous nurses, speech path
- Yes/no questions are your best friend!
- Don’t give up, don’t pretend to understand
- When all else fails, work through Maslow’s hierarchy of needs
Keep in touch!
http://media5.picsearch.com/is?x-it1FwobJGSsNDgUPRAR0hNi142nrjdVsOuFjXAwh8&height=189
http://3.bp.blogspot.com/_ZKzIOz7RVkY/SeACNhI698I/AAAAAAAAACI/G5wKc7AyOJI/s200/Key+word+%27TOILET%27.bmp
https://ecdn.teacherspayteachers.com/thumbitem/Low-Tech-Communication-Board-1500873671/original-126187-1.jpg








You must be logged in to post a comment.