Table of Contents
Written by Tiffany Taylor (RN) – editing team with The Nurse Break
This is to complement our very brief cheat-sheet guide for your cardiac nursing placement
If you are about to go on placement or start a job on a cardiac or cardiothoracic ward, this page will help you with key information that you should know. Please note, not all answers are provided to all questions as this article is intended to guide your learning. It is much more valuable to have you do the research on your own which will make you a better learner and in turn a better nurse. We have tried to ensure accuracy as much as possible.
Not All Cardiac Wards Are the Same…
First things first, not all cardiac and cardiothoracic wards are the same. Some hospitals have the two specialties split in separate wards. These are usually called a Coronary Care Unit (CCU) and a Cardiothoracic Unit (CTU), meaning your placement could be medical or surgical. Some cardiology specialties are split even further into cardiology (medical only) and CCU (surgical). Other hospitals have these services combined on the one ward, meaning your placement may be both medical and surgical in nature. Some hospitals will also have the “cath lab” on the same floor as the CCU to allow patients a smooth transition from angiogram to the ward or vice versa. The cardiac wards usually work closely with HDU and ICU to smoothly facilitate bed transfers and in some hospitals these areas are linked together to make a cardio and thoracic centre (CTC).
Some other articles you will enjoy
- For a comprehensive and systematic approach to assessment in ICU, read THIS POST
- For a guide to placement/grad year on a cardiac / cardiothoracics ward + free worksheet on cardiac pharmacology and main cardiac issues go HERE
- Cheat-sheet guide for your ICU nursing placement HERE
- Introduction to Cardiac Nursing Basics for nursing students
- The ultimate nursing guide to sepsis
- A cheat-sheet guide for your cardiac nursing placement
- The helpful complete guide to an Aged Care Nursing Placement for students
- 14 strategies for successful clinical placements
- Untangling nursing communication – “My patient can’t talk to me… Help!”
- Step-by-step explanation of nursing CPD
- Helpful list of proven graduate nurse tips!
- You MUST know about ACT-PINCHES (N) drugs
Cardiac Nursing Basics – The Anatomy of the Heart
Location and size of the heart
The heart is approximately the size of the average adult’s fist, roughly 12.5cm in length from base to apex. There is some variation in size depending on gender and heterogenic variation. It is conical shaped, hollow and surrounded by a protective sack called the pericardium. It rests within the inferior mediastinum with the base of the heart at the level of the third intercostal space approximately 1.2 cm right of the sternal midline and the apex at the level of the fifth intercostal space at the midclavicular line, approximately 7.5cm left of the sternal midline.
Something cool to think about – The heart beats so forcefully that it’s apex thumps against the thoracic wall. You can auscultate this with a stethoscope at the midclavicular line at the level of the fifth intercostal space or the point of maximal impulse (PMI). In some patients you will be able to palpate the apical impulse at the PMI, this can be a normal finding however if you can see the pulse without palpation this can indicate certain chronic conditions are at play. You’ll have to do your research to find out more there! Try starting with precordial impulses and their meanings.
The Heart Wall
The heart wall is made up of cardiac muscle fibres that are arranged in a spiral. There are three distinct layers Endocardium, Myocardium and Epicardium. Protective layers of the heart include the Parietal Pericardium and the Pericardial Cavity.
Chambers, Great Vessels and Valves of the Heart
There are four chambers of the heart which receive and pump the circulating blood. There are two atria located superiorly and two ventricles located inferiorly with a wall of muscle dividing the heart down the middle into left and right called the septum. Internally the right atrium is separated from the right ventricle by the right atrioventricular valve or the tricuspid valve. It is known as tricuspid because it has three “flaps” that come together to form a seal.
The left atria is separated from the left ventricle by the left atrioventricular valve or the bicuspid/mitral valve, again it is known by this name as it has only two “flaps” that come together to form a seal. The right and left ventricles are protected from blood pooling back from the pulmonary artery and aorta respectively by the pulmonary and aortic semilunar valves. As the name suggests, these valves are made up of three half-moon shaped appendages that come together to form a seal. I like to think of them like a few Chesire cat smiles that come together.

There are two grooves on the surface of the heart which carry the blood vessels that supply the myocardium. These grooves also mark the boundaries of the four chambers of the heart. The atrioventricular groove, also called the coronary sulcus sits under the atria and above the ventricles and encircles the heart. The anterior interventricular sulcus runs between the left and the right ventricles.
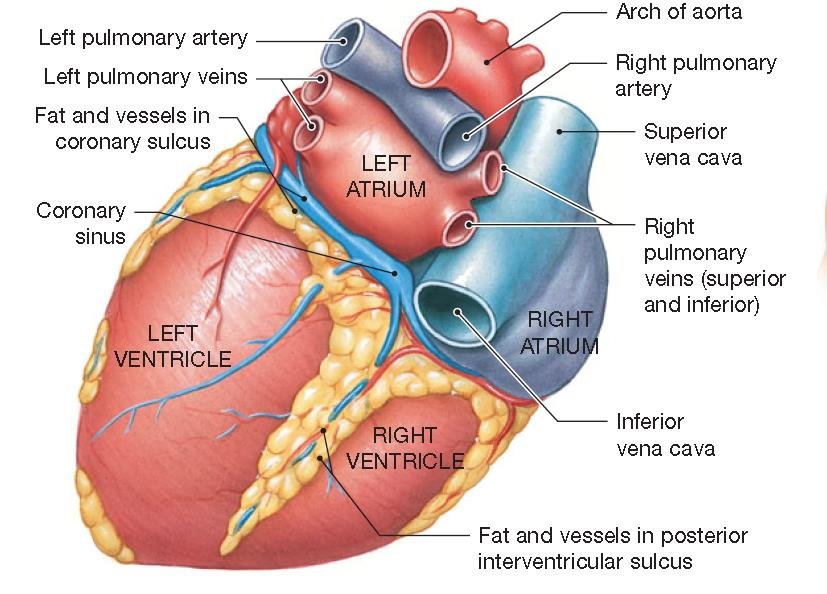
Reference drawing, courtesy of Kenhub
(https://www.kenhub.com), illustrator Yousin Koh. Accessed September 4th, 2020
The Pathway of Blood Through the Heart
The pulmonary and systemic circuits. Sometimes it helps to think of them as separate entities but be mindful to remember they both work together simultaneously. The pulmonary circuit receives oxygen poor blood returning to the heart from the body and delivers it to the lungs for oxygenation. The systemic circuit supplies the entire body with oxygen rich blood.
The right side of the heart is the pulmonary circuit pump. Oxygen poor blood returns from the peripheries via the superior and inferior vena cava and passed through the right atrium into the right ventricle through the tricuspid valve. The right ventricle then pumps the blood into the pulmonary trunk via the pulmonary semilunar valve and into the lungs to undergo gas exchange. The pulmonary veins then transport the oxygen rich blood back to the left atria.
The right side of the heart is the systemic circuit. Oxygen rich blood arrives in the left atria via the pulmonary veins and passes through the mitral valve or bicuspid valve into the left ventricle. The left ventricle then pumps the blood through the aortic valve and into the aorta. Oxygen rich blood is then distributed around the body where it undergoes gas exchange and returns into the pulmonary circuit.
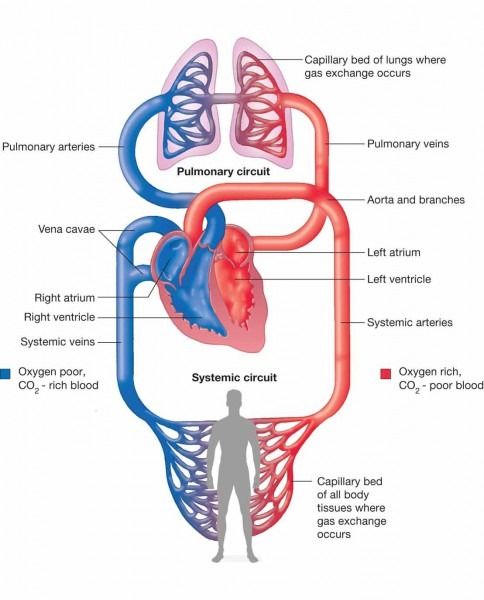
Reference drawing, courtesy of Kenhub
(https://www.kenhub.com), illustrator Yousin Koh. Accessed September 4th, 2020
The Coronary Arteries and Veins – How the Heart Gets Its Blood Supply
We touched on the coronary sulci before and how that is where the coronary arteries sit, allowing blood flow through the heart but let’s look at it in a little more detail.
The right coronary artery arises from the aorta near the right cusp of the aortic valve (displayed in the picture below). It lies across the right atrium and right ventricle with its major branches including sinoatrial and AV nodal, posterior descending, marginal and conus.
The left coronary artery arises from the aorta near the left cusp of the aortic valve (displayed on the picture below) and divides from the left main artery into two branches, these are called the circumflex and the left anterior descending arteries.
After passing through the capillary beds of the myocardium, the oxygen poor blood is collected and returned via the coronary veins. The path is the same as the coronary artery pathway with the exception of the blood being returned via the coronary sinus which sits within the coronary sulcus and draining into the right atrium. There are three veins within the coronary sinus. The great cardiac vein which drains from the anterior portion of the heart. The middle cardiac vein which drains from the posterior portion of the heart and lastly the small cardiac vein which drains from the right side of the heart. There are also several anterior veins which drain directly into the right atrium.
The Physiology of the Heart
It’s very easy to be completely overwhelmed by the physiology of the heart and all it’s electrical conduction and excitation events. The key here is to take it one step at a time and wrap your head around the basics before trying to move on.
Cardiac Muscle
Let’s go back to A&P 101 really quickly. Mitochondria are… THE POWERHOUSE OF THE CELL. We all remember! We also remember that oxygen exchange and ATP creation happens at the cellular level during cellular respiration within the mitochondria – oh yeah that Krebs cycle (TCA cycle) you had nightmares about before exams, turns out you do need it, but only a little!
So, 25% of cardiac muscle fibre volume is made up of mitochondria compared to about 2% in skeletal muscle. This means that the cardiac muscle fibres rely almost exclusively on aerobic as opposed to anaerobic respiration. This means that while skeletal muscle can contract for long periods even at an oxygen debt, cardiac muscle fibres cannot incur such an oxygen deficit and are unable to function at an oxygen debt.
Cardiac muscle is however adaptive when it comes to nutrients for energy and can switch metabolic pathways readily to derive ATP from glucose, fatty acids and lactic acid. This means that the main danger of inadequate blood flow to the myocardium is not a lack of energy but a lack of oxygen. Just in case you didn’t already thing that from the previous paragraph!
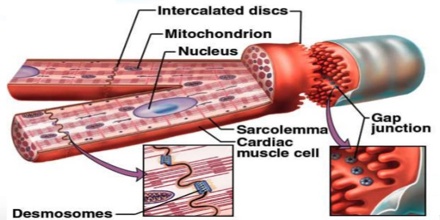
Cardiac muscle is striated and comprised on thick (myosin) and thin (actin) filaments that interact with on another to form a contractile response in the presence of calcium. Cardiac muscle is short, fat, branched and interconnected with each fibre containing one or two large, pale, centrally focused nuclei. The intercellular spaces are filled with a loose connective tissue matrix containing numerous capillaries. This matrix is connected to the fibrous skeleton of the heart which acts as both a tendon and an anchor for cardiac cells to pull and exert force against.
Cardiac cells are interconnected at junctions called intercalated discs. These discs contain anchoring desmosomes and gap junctions which aid in the propagation of action potentials and allow the cells to contract in unison. This also aids in allowing the electrical potential of an action potential to spread. The entire myocardium functions as a single unit known as a functional syncytium due to the electrical coupling of cardiac cells by gap junctions.
Mechanism and Events of Contraction
For a mechanical event to occur, there must be an electrical input. For example, think of when you turn the lights on at home. You flick the switch and the light turns on but there had to be an electrical potential that traveled from the switch and arrived at the light to propagate the bulb illuminating. This is essentially what happens in cardiac muscle to generate a contractile response. This electrical potential is called an action potential.
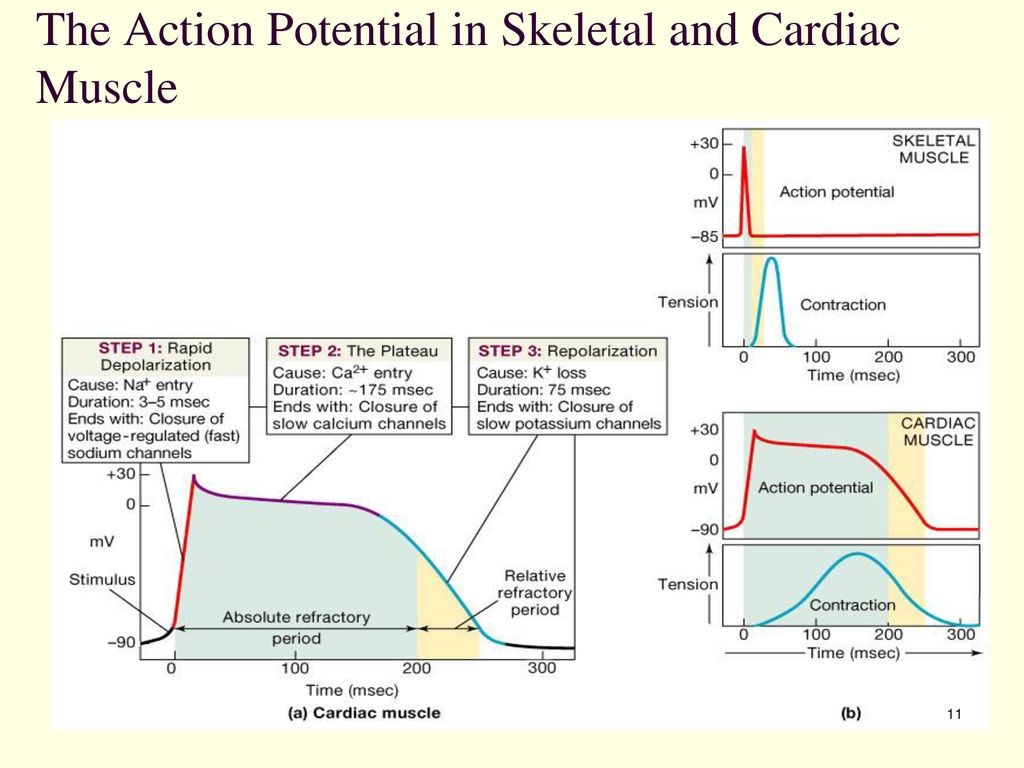
An action potential represents a change in intracellular electrical potential (mV) measured over a set period of time. The action potential is initially negative in relation to cations and anions across the cell membrane such as sodium (Na+), calcium (Ca2+) and potassium (K+). The resting membrane potential (RMP) or the point at which the cell is at rest or relaxed of a cardiac muscle cell is -90mV. Skeletal muscles cells are at rest at -70mV. Cardiac cells are therefore considered more stable at rest and harder to stimulate.
The point at which an action potential will always occur is called the threshold potential and occurs at -50mV. At this point the membrane potential becomes more positive and depolarisation occurs, secondary to a rapid sodium influx into the cell. The peak of an action potential lies at +30mV and will plateau at this point due to a slow calcium influx into the cell. Synchronicity of the atrial contraction is supported by the slow influx of calcium, allowing time for the atria to be fully electrically stimulated before the ventricles. The cell then returns to its RMP through the moderate influx of K+ out of the cell.
The action potential itself initiates the cycle of depolarisation and repolarisation in the cardiac cells. This cycle has three phases which will be covered next. There are also two important periods that ensure the protection and optimal function of cardiac muscle cells, the absolute refractory period and the relative refractory period.
Phase 1: Rapid Depolarisation
Voltage gated sodium channels open at -50mV resulting in a rapid influx of positively charged ions (cations) into the cell. The cell in turn becomes more positive and at the end of the influx the cells membrane potential is at +30mV. The duration of this phase is 3-5msec.
Phase 2: The Plateau
Once the membrane potential has reached +30mV, the voltage gated sodium channels become closed and incapable of opening. These channels will remain closed until the membrane potential becomes less than or equal to -60mV.
Voltage gated calcium channels begin to open and allow a slow influx of calcium into the cell. Sodium is also actively transported out of the cell essentially acting to balance each other out. This maintains a prolonged plateau phase
The calcium is directly responsible for excitation contraction coupling (ECC) where calcium interacts with think filaments within the cardiac muscle cell. The thin filaments then interact with thick filaments which generates a subsequent contraction.
Phase 3: Repolarisation
Slow voltage gates calcium channels being to close and voltage gated potassium channels open allowing a moderate efflux of potassium out of the cell. The cell returns to RMP.
Absolute Refractory Period (ARP)
A period lasting approximately 200msec where the cell membrane can not respond to a second electrical stimulus as a direct result of open or closed voltage gates sodium channels, meaning they are not capable of producing another rapid influx by opening and therefore are essentially inactivated.
Relative Refractory Period (RRP)
Following immediately post the ARP sodium channels are closed and capable of responding to a second stimulus. If the second stimulus is strong enough it will lead to the propagation of a second action potential.
Excitation and Electrical Events
Myocardial cells electrophysiology has four unique characteristics.
Automaticity
Pacemaker cells which make up 1% of cardiac muscle tissue can spontaneously generate an impulse due to an unstable RMP propagating an action potential. Automaticity is the term used for this self-excitation and includes the maintenance of rhythmic activity.
Excitability
Refers to the cellular response to natural or artificial stimulus. Cardiac cells are excitable because of the constant ion exchange across their cell membranes. The degree of excitability is directly related to the cardiac cycle and refractory periods.
Conductivity
The transmission of an impulse from cell to cell including those impulses strong enough to create a wave of excitation that is propagated to the whole of the myocardium.
Contractility
The term used to describe the ability of muscle fibres to shorten when electrically stimulated. It is a mechanical response to electrical activity.
Note: Electrical activity always precedes mechanical.
It’s important to understand that the ability to depolarise and contract displayed by cardiac muscle is intrinsic meaning that it is a property of the heart itself and does not depend on external or extrinsic nerve impulses.
Cardiac Conduction System
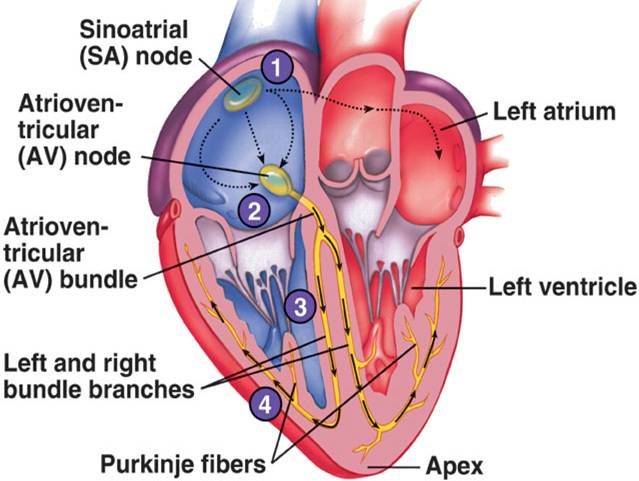
Sinoatrial (SA) Node
Where the superior vena cava meets the right atrial tissue mass is where the SA node is located. Measuring around 10 – 20mm and oval shaped, the SA node is the hearts main pacemaker. At rest it initiates 60 – 100 beats a minute.
Impulses travel from the SA node through to the left and right atria. Within the right atria there are three groups of internodal tracts. Anterior; Which enters the anterior portion of the atrioventricular (AV) node. Middle or Wenkebach; which enters the superior margin of the AV node and posterior or Thorel Tract; which reaches the lower portion of the AV node.
To achieve simultaneous contraction between the right and left atria, the impulse travels through the left atrium via Bachmann’s Bundle extremely fast.
Atrioventricular (AV) Node
The AV node is positioned in the right atria between the coronary sinus and the tricuspid valve’s septal cusp. Measuring around 3 – 6 mm and disc shaped, it consists of interlacing conduction fibres. The AV node conducts atrial impulses through to the ventricles with an approximately 0.4sec delay on the way to allow the ventricles to fill with blood while the atria complete their contraction.
There are three regions of the AV node. The upper portion known as the Atrinodal Junction where the anterior, middle and posterior interatrial tracts meet. The AV node receives its blood supply from the RCA in 90% of people and the Circumflex in 10% of people. The AV Node Proper where conduction is delayed due to the structure of the fibres in this area. Rhythms that originate in this area are known as junctional rhythms and lastly the Bundle of HIS which deserves its own paragraph.
Bundle of His (BOH)
The BOH is located on the right side of the intra atrial septum and extends downwards and leftwards entering the inter ventricular septum. It is the sole muscular connection between the atria and the ventricles. Rapid conduction occurs through the BOH, which divides into the right and left bundle branches which extend down either side of the intra ventricular septum. Conduction velocity is greater in the left than the right which gives the larger muscle of the left ventricle the extra time needed to contract in unison with the right ventricle. The BOH has an intrinsic firing rate of 40 – 60 beats per minute.
Right Bundle Branch (RBB)
The RBB is a well-defined long fibre that travels along the right side of the interventricular septum until it reaches the anterior papillary muscle at the apex of the right ventricle. From here it divides into the Purkinje system which spreads over the right free wall and the right ventricular septum.
Left Bundle Branch (LBB)
The LBB disperses almost immediately into a fan like structure. There are two main divisions. The Anterior Superior Fascicle which is long and thin and located below the aortic valve within the left ventricle outflow tract. It courses along the left inter ventricular septum to the anterior papillary muscle and to the apex of the left ventricle. The Posterior Inferior Fascicle is short and thick, situated mostly in the left ventricle inflow tract. It follows the left ventricular inflow tract to the posterior papillary muscle and posterior inferior wall of the left ventricle.
Purkinje Fibres
The Purkinje fibres are a diffuse muscle fibre network believe to lack nervous supply that transmit impulses quicker than any other part of the conduction system. The Purkinje system will become a pacemaker site when the SA and AV nodes fail or if impulses are blocked in both branches. The automatic firing rate of the purkinje fibres ranges from 20 – 40 beats per minute.
Electrocardiography (ECG)
ECG detects and records electrical impulses on the surface of the body that are generated from the myocardium in relation to electrical flow through the heart.
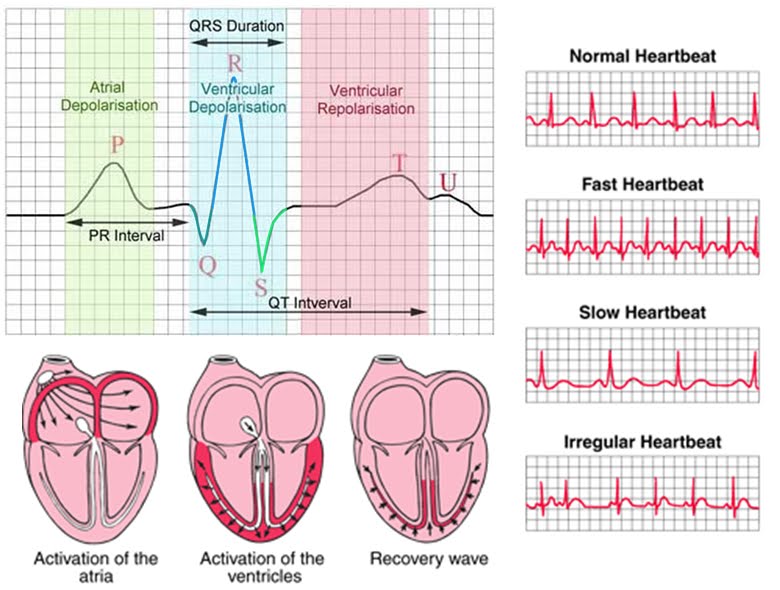
P Waves
P waves represent a depolarisation wave through the SA node and atrial precontraction. They are a small raised rounded wave that precedes all other recorded electrical impulses on a normal ECG.
QRS Complex
QRS Complex represents the depolarisation of the ventricles pre contraction and denotes the different size of the ventricles through its shape. Atrial repolarisation happens during this period but is hidden by the more powerful QRS complex.
T Waves
T waves represent the repolarisation of the ventricles which is slower compared to depolarisation, therefore making the wave more spread out than the QRS Complex.
PR Interval
PR interval represents the period of time from the beginning of atrial depolarisation to ventricular depolarisation inclusive of the atrial contraction.
Q-T Interval
Q-T Interval represents the time from the beginning of ventricular depolarisation to the end of ventricular repolarisation inclusive of ventricular contraction.
There are other parts of an ECG such as the PR and ST segments but lets just stick with the basics on this one.
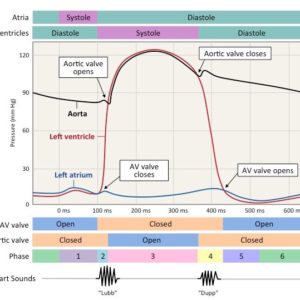
Cardiac Cycle
The cardiac cycle is the description of contraction and ejection events occurring within one beat of the heart. It can be broken down into periods of systole and diastole. The cardiac cycle is less than 0.80 seconds from the onset to the completion.
Even though this section is relatively small, it pulls together a lot of the previous reading and explanations, so stay with me here because we will be referring back to terms already mentioned.
Systole
Isovolumetric Ventricular Contraction
Isovolumetric Ventricular Contraction happens in response to ventricular depolarisation creating tension in the ventricles. This phase begins shortly after the onset of the QRS on ECG. The AV valve closes here creating the S1 heart sound on auscultation related to turbulence of blood flow around the valve leaflets. The aortic and pulmonic valves are closed completely during this phase. The volume of blood in the ventricles is constant and aortic pressure is about 80mmHg. Ventricular muscle fibres contract on a constant volume of blood to increase pressure which then rises steeply.
Rapid Ventricular Ejection
Rapid Ventricular Ejection happens as the ventricular pressure increases past that of the pulmonic and aortic valves. The aortic and pulmonic valves open with the ventricles ejecting blood into the aorta and pulmonary circulation. Ventricular volume decreases sharply, the atria begin filling. This phase also includes the beginning of ventricular repolarisation which is represented by the T wave on ECG.
Diastole
Isovolumetric Relaxation
Isovolumetric Relaxation is when the ventricular pressure falls below the pressure in the aorta and pulmonary artery. The drop in pressure causes the pulmonic and aortic valves close and due to the turbulence of blood flow around the valve leaflets, the S2 heart sound can be heard on auscultation. Ventricular pressure continues to fall rapidly as the ventricles relax. Atrioventricular valves remain closed in both ventricles and as blood fills the atria during atrial diastole.
Ventricular Filling
Ventricular Filling happens when the atrial pressure is greater than the ventricular pressure and the AV valves open, allowing passive blood flow into the ventricles. An S3 heart sound may be heard here. Aortic pressure slowly falls and 80% of ventricular filling occurs. This can be seen on ECG by the isoelectric line.
Atrial Systole
Atrial Systole occurs slightly after the beginning of the P wave. This last phase also coincides with ventricular diastole and is when the atria contract in response to atrial depolarisation. This is known as the ‘atrial kick’ and contributes 20 – 30% of ventricular volume and pressure. Atrial relaxation occurs after this kick or ejection and the AV valves close. S4 heart sound may be heard during this phase. Pressure in the aorta continues to fall as the ventricles being to depolarise.
The cycle then starts again.
Assessments that will indicate the cardiac cycle is occurring correctly include the presence of a strong and regular palpable pulse, a blood pressure within acceptable ranges and normal heart sounds.
Source: https://ib.bioninja.com.au/standard-level/topic-6-human-physiology/62-the-blood-system/cardiac-cycle.html
Cardiac Output
Cardiac output (CO)
Cardiac output (CO) is the amount of blood pumped each minute from the left ventricle into the systemic system. Stroke volume (SV) is the volume of blood ejected from the left ventricle with each beat. Heart Rate (HR) the number of heart beats per minute. Normally CO ranges from 4-8 litres, depending on a person’s body size. The heart will only pump as much blood as it needs to meet metabolic requirements.
CO = SV x HR
In a resting adult SV averages 70mls and HR 70, resulting in a CO of 4900mls/min or 4.9L/min.
SV is determined by three factors;
Preload
The ventricular volume and pressure at the end of diastole. Preload determines how much cardiac muscles fibres are stretched during diastole, which in turn will affect contractility. Therefore, an increase in venous return will increase ventricular end diastolic volume and result in a more forceful systole.
Afterload
Also called systemic vascular resistance (SVR) is the resistance the ventricle must work against to eject blood during systole. This resistance depends on arterial blood pressure, valve characteristics, ventricular size and wall thickness. Diastolic blood pressure only provides a rough index of afterload.
Contractility
The ability of the ventricles to contract which depends on how much the cardiac muscles fibres are stretched at the end of diastole. The more the cardiac muscle fibres are stretched, the more forceful the contraction, causing larger amounts of blood to be ejected with greater force. This phenomenon by which the length of cardiac muscle fibre determines the force of contraction is referred to as Starlings Law of the Heart.
In a healthy heart, SV and HR work together to control CO. If SV decreases, HR will increase to maintain CO. IF the heart is damaged due to ischemic heart disease, valvular disorders or myocardial necrosis, CO will drop because ventricular filling time is reduced. This also occurs if HR is too high.
The amount and viscosity of blood also helps to regulate SV and therefore CO. The normal viscosity of blood results in part from red cell content and the amount of plasma protein. Increased viscosity due to dehydration for example will cause increased afterload. If blood volume is decreased through bleeding or dehydration, venous pressure will fall and so will venous return. Ventricular filling drops and CO is reduced.
The Ejection Fraction is the ratio of blood ejected from the left ventricle per beat (SV) to the volume of blood in the left ventricle at the end of diastole.
Regulation of the Heart
The Autonomic nervous system has two branches, the sympathetic and the parasympathetic and these dually innervate muscle to maintain homeostatic function.
The sympathetic nervous system has pre and post ganglionic nerve fibres which innervate all areas of the heart. These nerves originate in the spinal cord between the first thoracic and second lumbar vertebrae. The neurotransmitter that activates beta receptors on post ganglionic nerve fibres is noradrenaline. When stimulated sympathetic fibres increase heart rate and the strength of cardiac contractile responses.
Parasympathetic fibres arise from the vagal nerve which originates from the medulla. These fibres primarily innervate the SA and AV nodes. The neurotransmitter acetylcholine activates muscarinic receptors that lie on the post ganglionic nerve fibres. Stimulated parasympathetic fibres slow the heart rate and conduction velocity of the AV node. Parasympathetic effects are mainly supraventricular.
The heart also has sensory/afferent nerves. Cardiac nerves which arise in the ventricles, pericardium and coronary arteries connect with the central nervous system, relaying the sensation of pain.
Other readings for you
- A cheat-sheet guide for your cardiac nursing placement
- A cheat-sheet guide for your ICU nursing placement
- 14 strategies for successful clinical placements
- Untangling nursing communication – “My patient can’t talk to me… Help!”
- Step-by-step explanation of nursing CPD
- Helpful list of proven graduate nurse tips!
- You MUST know about ACT-PINCHES (N) drugs
References
Berman, A., Snyder, S. J., Levett-Jones, T., Dwyer, T., Hales, M., Harvey, N., . . . Reid-Searl, K. (2018). Kozier and Erb’s Fundamentals of Nursing [4th Australian edition]. In: Pearson Australia.
Betts, J. G. a., Desaix, P., Johnson, E., Johnson, J. E., Korol, O., Kruse, D., . . . Young, K. A. (2013). Anatomy & physiology: OpenStax College, Rice University.
Kroeker, C. (2018). Cardiovascular System: Anatomy and Physiology. Cardiovascular Mechanics, 1-17.
Loukas, M., Sharma, A., Blaak, C., Sorenson, E., & Mian, A. (2013). The clinical anatomy of the coronary arteries. Journal of cardiovascular translational research, 6(2), 197-207.
Magder, S. (2016). Volume and its relationship to cardiac output and venous return. Critical care, 20(1), 1-11.
Peate, I., & Evans, S. (2020). Fundamentals of anatomy and physiology: For nursing and healthcare students: John Wiley & Sons.





You must be logged in to post a comment.