Table of Contents
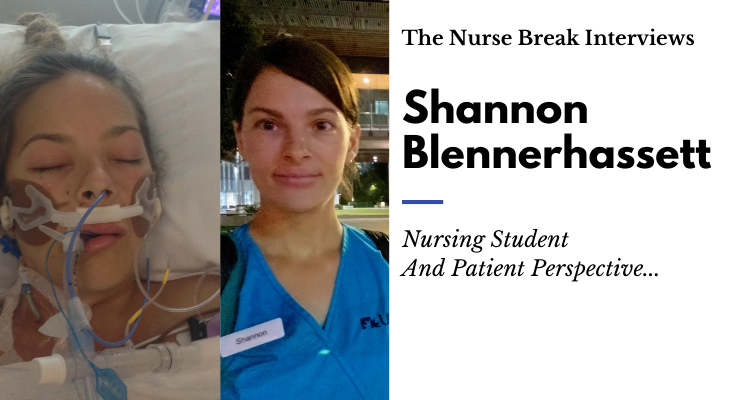
In 2018, Shannon Blennerhassett underwent a simple procedure at her G.P’s to insert a contraceptive device. By 9 pm that night, she was being rushed to the Emergency Department at SCUH. The patient perspective.

I am a 28-year-old mother of 3 young children. I grew up in Brisbane but have lived in Perth, WA, Dalby in QLD and now I live on the Sunshine Coast. I had many jobs but never felt passionate about a career option. Now that I have found nursing I can’t believe I didn’t realise this was where I’m meant to be sooner.
How it begun
I had just had my 3rd child and wanted a contraceptive device. It was recommended to me by my GP to have a Mirena inserted and I agreed. My son was 6 weeks old when I had the procedure. As soon as I got home from the GP I was filling maternity pads and passing enormous blood clots.
I went to the Emergency Department at 9 pm and had an ultrasound to determine whether the Mirena had indeed perforated my uterus. There were lots of people in the room and there was no definitive answer.
I stayed in the emergency overnight and was closely monitored. In the morning I had lost a significant amount of blood so the decision to undergo a laparoscopic surgery was made.
After the balloon insertion, I was recovering on a surgical ward, however, when I sat up in bed coagulated blood gushed out from me, within minutes my bed was completely filled with blood. I hit the buzzer and soon a code blue was called, and my room filled with doctors and nurses. I remember vomiting, shaking uncontrollably and giving consent for massive blood transfusion to begin while they prepped for another surgery. My partner was called, and he brought my 3 children to the hospital and was told he had a few minutes to go in and say goodbye.
“It really was a traumatic thing you know, waking up in a pool of your own blood. I had a six-week-old baby at the time, so I wasn’t able to look after him or feed him. The experience in itself was horrible, but one of the things I took from it was how incredible the doctors were obviously for their clinical skills, but the nurses for their people skills and their communication is the main thing that I remember from it.”
The next time I woke up I was in the ICU and was intubated

The next time I woke up I was in the ICU and was intubated, I was told that they still had not been able to find the bleed and that I had to have a 3rd surgery. I was told it would likely result in a hysterectomy. I gestured that I wanted to hold my baby and I was allowed to do so. I said goodbye to my family once again.
After the third surgery, I stayed in the ICU a total of 5 nights where I was cared for by an incredible group of nurses. I still remember the names of my favourites and a new graduate nurse who had just started. I was told that in total I received 18 units of blood and that when I went into haemorrhagic shock my HB was around 40.
After ICU I went to the ward where I stayed for several weeks on IV Abs, more blood and recovering. The nurses took the time to hear my story and help me process what had happened.
Tell us about some of the positive and negative moments
The positive moments were when the ICU nurses braided my hair to stop it from matting, reassuring me when I had bad dreams, understanding the trauma of what had happened and helping me to feel safe.
“I still remember there was a graduate nurse and it was her first shift on her own in ICU and she was just incredible, really attentive and made me feel very comfortable.”
A negative was a nurse who when I initially buzzed during the haemorrhage came to the door and said, your nurse is on a tea break. I said I was feeling really light headed and she said not to worry and left. In reality, I was bleeding out internally, I take this as a lesson to always listen to your patient’s concerns, do a set of vitals… Because my deterioration went unrecognised. I often think about what my observations would have been at that point.
If there’s one thing you’d like to pass on to members of the public, what would it be?
Ask your nurse questions, be actively involved in your care and have a sense of agency. Having knowledge about your health status enables you to be an advocate for yourself.
Has the patient perspective changed your view on what happens in a hospital?
Definitely, I can understand from both sides now. It has made me a more empathetic nurse. I think all lived experience does. Last year I lost my dad suddenly to cancer. It gave me a whole new respect for palliative care. I think all nurses are shaped by our life experiences. For me, I have been the tubed patient, I have been the mother of a sick child, scared and consumed with worry. I have been the daughter of a dying patient, in complete despair.
What were some of the longer-term impacts?
For my time in the ward and when I got home, I initially woke up in a panic thinking that I was bleeding again. I would feel so light-headed and panicky, it took time to ground myself and remember that I was safe and that it wasn’t happening again.
I lost trust in the medical profession and was hesitant in excepting medications. This insight allows me now, having healed emotionally, to realise why some patients behaviours are the way they are. It allows me to be a more patient nurse and to accept that each patient has been through their own ordeals to end up in the hospital. Which is generally not a place anyone wants to be.
“I’m so grateful to live in Australia and have access to the level of healthcare we have. I feel like if this happened anywhere else, I would have died. One of the senior gynaecologists performed a second surgery and managed to stop the bleeding, and I spent a few weeks recovering before I went home.”
After the life altering experience, Shannon began studying Nursing Science at USC (University of the Sunshine Coast).

Do you have a story or is someone you know potentially keen to share theirs? Contact us!





You must be logged in to post a comment.