Table of Contents
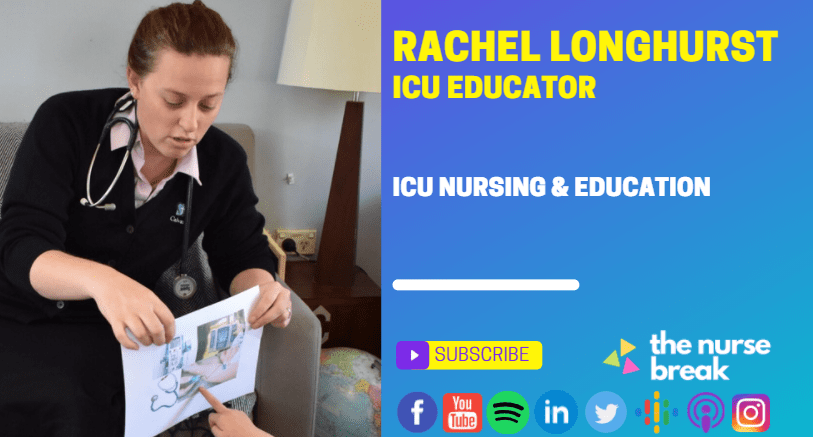
Meet Rachel Longhurst! She is an ICU Nurse Educator from one of Canberra’s Public Hospitals, who talks openly about her love of all things ICU and Education!
Part 1 of our interview with Rachel presents her nursing journey so far, including achievements with the Australian College of Critical Care Nurses, and what she gets up to during a typical day in her role as Clinical Nurse Educator.
Background
What impact has COVID-19 have on you as a nurse educator?
The COVID-19 pandemic has been an interesting time to be in healthcare. I remember one of our consultants saying to me in March last year, that it was like standing on a beach, a tsunami imminent and not knowing how high the waves would be and how far they would go. And that was apt. Regardless of what was coming, we had to prepare for it as if the waves were going to be unimaginably high. I’m not sure I’ve ever worked as hard as I did in the three month period between March and May last year. Except for maybe in the last 5 weeks when the earth quaked and the tsunami warning came again. And this time it was more real as COVID was being transmitted within the community in the ACT.
Healthcare professionals have been taught to base clinical decision making on evidence from rigorous studies. It usually takes 10-17 years for research to find its way into clinical care. With the first wave of COVID we didn’t have a great deal of evidence and we didn’t have that timeframe. Guiding organisations were saying ‘we need to wait for some kind of evidence before we can publish guidelines’ and many of our clinicians were in a frenzy of fear because they were being bombarded with images and stories on social media coming in from overseas.
They wanted and needed guidance on how to care for these confirmed and suspected patients now. This resulted in a lot of hospitals and organisations just ‘doing their own thing’ in the initial phases. I was no different. There was a weight of responsibility on many of us. I wanted staff to feel somewhat safe, I wanted staff to feel they had a process to follow. I tried really hard to make sensible decisions based on the best possible information available or the nearest possible historical information. And it’s nice to know that many of these sensible decisions have been backed up by the evidence that is now emerging.
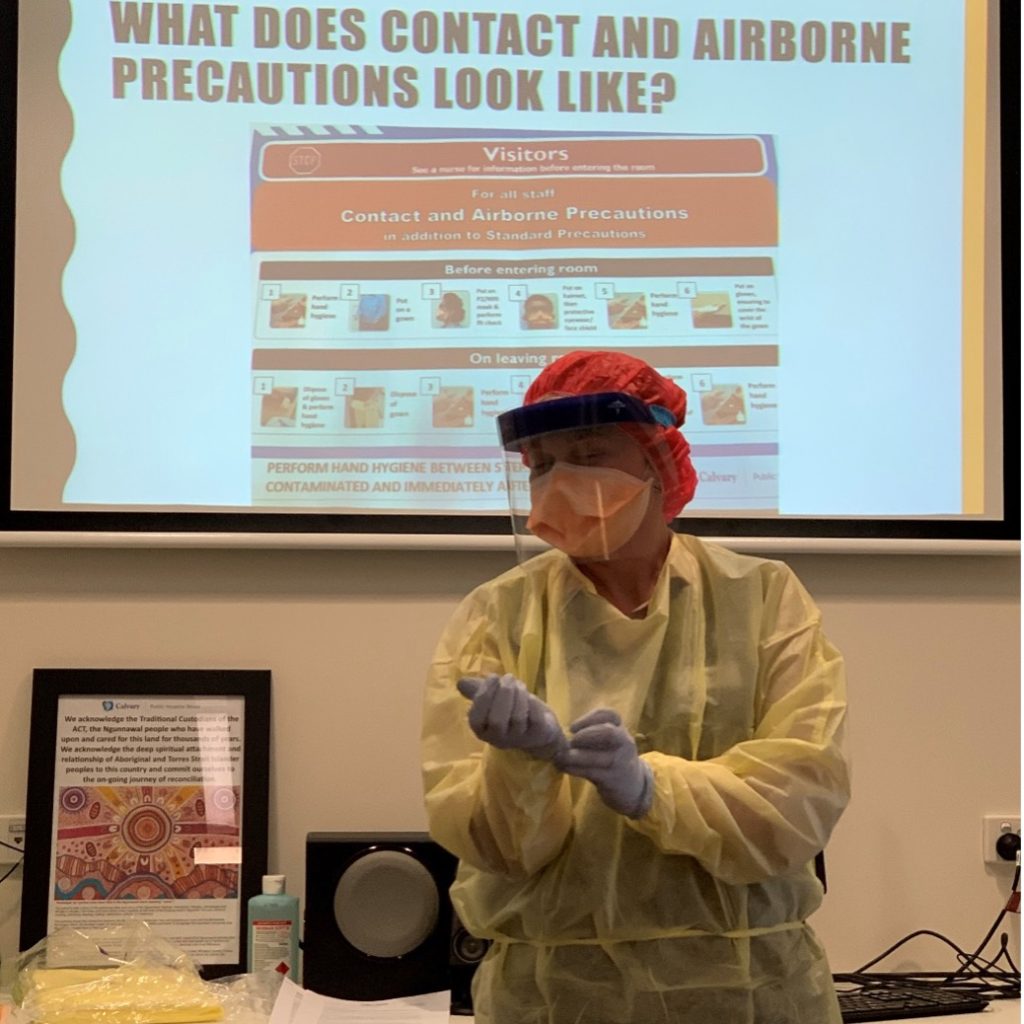
PPE training was an immediate priority as COVID emerged. I laugh now, because our annual fit check and hand hygiene training are not usually well attended voluntarily. We had over 90% of our ICU staff voluntarily attend PPE training within a 1 week period as COVID emerged. And that PPE competency has been maintained. It gives a lot of weight to Knowles’ Adult Education Principle of relevancy and self-identified learning needs. Fear also happens to be a pretty good motivator.
As the pandemic commenced, from an education perspective we knew that we needed to come up with plans for how we would manage COVID patients, especially how we would intubate, ventilate, extubate, resuscitate and prone these patients. And then we had to attempt to train all our staff under a ‘no group activities’ mandate, in a way that adhered to social distancing requirements.
There was a huge amount of workforce planning that was undertaken initially. And then under-taken again with the emergence of the Delta variant. In the very early days the government promised everyone who needed it, an ICU bed. This involved projecting where ICU beds could be established if required and procuring large volumes of equipment. But the most important resource is, of course, the human resources and these are much harder to come by. It takes about 12 months to develop a foundational critical care nurse, and about three years to create a proficient one.
How did you enter into nursing and why?
I entered my nursing degree straight out of high school – quite naively in hindsight (laughs). I actually wanted to study, and got accepted into, forensic science. This was based on my early love for Patricia Cornwell novels. My mother can still tell you all about the time I dissected our family’s dead goldfish. However, I decided that biology was a stronger point than chemistry and made a late change to Nursing. A lot of people over the years have asked ‘why nursing’ and I think subconsciously it had to do with the fact that in my final years of high school I had a couple of close relatives die in hospitals after a period of illness. I can still vividly remember visiting them in that space, the powerlessness I felt and, ultimately, the loss.
I enjoyed a lot of my placements during my undergraduate degree. After my first placement I was going to be a community nurse, after my paeds placement, I was going into paediatrics. However, it was my last placement in critical care that really got under my skin. Based in a combined ICU/HDU/CCU I saw a lot of interesting things, but more than that, I had a couple of preceptors who took me under their wing and made an interesting placement amazing. They opened my eyes to how much there was to learn (and how much I still had to learn).
Once I graduated, I obtained a position as a new graduate and after completing a medical and surgical rotation I was able to return to critical care, to the unit that had sparked my interest and those preceptors became my colleagues. Since then, though I have moved between hospitals, I have not moved out of the critical care space. I’ve spent some time in various HDU/ICUs, CCU, and ED.
One of the most wonderful things about nursing is that it has so many specialties and niches – I was lucky I found mine early on.
– Rachel Longhurst
Can you talk us through your journey from Student Nurse to ICU Educator?
I was fortunate as both a student and new graduate nurse that I had some passionate and invested nurses take an interest in guiding me through my early career – people who I call my friends still to this day. I had a great preceptor who became a mentor, someone who encouraged me into the education space with enrolled nurses, which gave me an opportunity to obtain my Certificate IV in Workplace Training and Assessment.
Being involved in the training of others helped me grow myself significantly as a clinician. From there I was able to do some clinical facilitation with registered nursing students and start to build a portfolio in education. I worked as a clinical development nurse for a number of years supporting junior staff on the floor, and then, after I returned to work following my second lot of maternity leave, I applied for and was successful in gaining the Clinical Nurse Educator role – something I saw as my dream job in nursing.
There are many challenges and hurdles as you progress throughout your career. The ‘culture’ of a shift, ward or organisation you might find yourself in, the senselessness and randomness as you face mortality, the steep learning curve every time you transition to something new. These are the things that university cannot prepare you for.
Nursing Education
Why do you love nursing education?
I love my job because it allows me to work with people who can influence change at the bedside (where I feel it really matters – to patients and families). I can have a direct impact on quality and safety through education, quality improvement and change management. No two days are the same, and there is always something to challenge me. I’ve seen what good investment into people’s professional growth is able to achieve. When you invest in people they are so much more likely to pay that investment forward to the next lot of students or junior staff, because they know what they got out of it. And this goes an amazingly long way in supporting good culture.
What makes a great nursing educator?
There are lots of things that go into making a great nurse educator. Leadership skills including good interpersonal skills, emotional intelligence, and capacity for driving change; clinical knowledge and skills, including the capacity to troubleshoot; understanding of adult education and how to provide it, this includes an understanding of education theory, teaching clinical reasoning, and using of a range of instructional methods to deliver teaching; management skills including data management, strategic planning and evaluation; and finally, a mindset of continued education and growth for themselves.
Have you experienced ‘bad’ nurse educators over the years?
Most often, advanced nursing roles go to great clinicians, and while these roles require clinical knowledge and skill, the roles themselves are much more about leadership, education and/or management. These are things that nurses are not always taught how to do well, things that nurses aren’t necessarily held to account to when they are working clinically. There are people who aren’t suited to education (and the same is true of other advanced roles) and this occurs for a variety of reasons. This is why it’s so important that when areas are recruiting they are not just interested in filling a position, but interested in finding the right person and right fit for the role.
No one should do a job like this just because they like the hours and get an office. And no one should stay in a job once they lose the spark that motivated them to do that job in the first place.
What things do you do behind the scenes as a nurse educator that people may not realise?
On average, I probably only spend about one fifth of my time ‘clinically visible’. I am fortunate to have clinical development nurses who work in my team, they spend much more time working one-on-one with our staff conducting upskilling and any required competency assessments. So when people can’t see me, things I might be doing include:
Recruitment
I am involved with recruitment in the unit, particular the recruitment of our transition to critical care nurses. I invest a lot of time into this process because I believe it’s important to bring the right people into a foundational training program. I also sit on interview panels for our level 1 and 2 registered nursing positions. The interview process is a good place to ensure people are who they say they are on paper.
Orientation
I oversee the orientation program for all new nursing staff and our nursing students within the unit. This is another process I try to get right – give people what they need to begin with and you set them up for success.
Formal Education Programs and Delivery
We run a number of formal programs within our unit alongside a regular inservice program. A great deal of time has gone into developing our formal programs and now, into maintaining and updating these. There are study days within these programs, which are a full day of teaching. There is a lot of planning and preparing involved in any education delivery I do. For example, for every hour long presentation I deliver there is usually about 10 hours worth of work in researching and putting it together. There is also a component of marking within our formal programs and they take me about an hour per module to complete.
Professional Advancement & Post-Grad Support
The ACCCN advocate that ICU’s should have between 50-75% of their staff with post graduate qualifications. I assist and support our PG students to complete their practical assessments and with any written assessment support they require. Other professional development support includes mentorship, reviewing CVs and cover letters, and guidance for interview preparation.’
Policy & Procedure
I oversee our local policy and procedure development and review. I believe in having up to date, evidence-based policy and procedures available to guide staff.
Clinical Incident Review
I am involved in the review of clinical incidents, RCAs, identification and rectification of system issues, and facilitating incident debriefs.
Intra-Hospital & External Commitments
Within the hospital I am involved in a number of committees including those relating to the national standards, am a trainer for formal hospital-wide programs, including basic and advanced life support, Clinical Supervision (for guided reflection), and as a trainer for our Speaking Up for Safety program. External to the hospital I sit on a territory-wide educational working group and am involved with the Australian College of Nursing, in particular the ACT/NSW committee.
In the early days there was the need to plan to rapidly upskill non ICU staff for the event that they might end up caring for ICU patients during the pandemic. We ran training days for ward nurses and theatre nurses. The hospital encouraged those interested to take up the online MedCast upskilling courses and completion of this was mapped in a spreadsheet. We developed bedside manuals and educational materials to have available for non ICU nurses that might find themselves suddenly in an ICU. Again, at the moment, we are working through the complexities of managing and potentially sustaining surge capacity.
Change Management
Among the first wave of COVID my 2020 cohort of transitions commenced their program in the ICU. We normally provide a graded and supportive program. It was the first time I felt I could promise nothing. If things went badly, I knew they would be managing very sick patients – likely with little support. And that was a hard thing for me to swallow. It did however, tweak the way I ran the program this year, meaning that my 2021 cohort had some changes to their program to ready them for our current situation.
This is another time-consuming element of my role, and this is most often done under the guise of quality improvement. The aim is to develop and implement strategies for how we may make things better within the unit for patients and more efficient for staff. I also assist and guide staff who may wish to undertake their own QI in the unit.
Admin
Like any job, there is a great deal of admin that is involved with my role each month – data collection and entry, reporting, rostering for the clinical development nurses, a monthly education newsletter, the maintenance of an allocation tool to help team leaders safely allocate for their shifts, inservice calendar generation and of course, an endless supply of emails to keep on top of.
In 2010 you moved from Private to Public ICU nursing. What were some of the differences you noticed between these two settings?
I started my career in the private sector and absolutely loved the team I worked with. I learnt a lot, fast. At the time we didn’t always have an ICU doctor on site, so there was a high expectation on the nursing team to identify concerns early and to escalate at all hours of the day, directly to consultants. I learned the importance of good communication, accurate assessment and re-assessment following interventions, and the importance of advocacy in patient safety. I learned autonomy and a strong foundation for critical thinking working in this environment, and I am grateful to this day for that experience.
My move to the public health system was spurred mainly by my decision to undertake postgraduate study. My local program at the time required placements in both public ICUs and EDs, which my private-sector employer was unable to support at that time. Once I completed the postgraduate studies I made the decision to stay in the public system due to the clinical educational opportunities that were available there.
I think there are pros and cons of both systems, but for me, it’s about working in an environment that sustains positive culture and puts the safety of patients and staff first. These things are achievable in both sectors under the right leadership. Likewise, they can be missing in both sectors when the pressures of time and money overshadow or dictate decision making.
What are the myths or common misconceptions that you want to debunk about nursing educators?
I once went to a social function and someone asked me what I did for a living. When I said I was an ICU nurse educator, I was asked, ‘What do you do all day? Teach people to wipe bums? Don’t they go to nursing school for that?’. It was such a lesson in self-restraint. Generally, I try not to take too much offence to general public misconceptions about nursing and nursing education. I tell people that it’s a job focused on ongoing learning for staff and quality control within the system. Deep down the truth is that I hope most people never have to find themselves in a position where they learn what the role of a ICU nurse is and why the role of a nurse educator in this space is so important.
What does a typical day look like for you?
I’m not sure there is any such thing as a typical day! However, I try to start my day by rounding in the unit – checking in with the management team, shift team leader, the staff, in particular our transition staff or students rostered, and get a feel for the patients that are in the unit, their acuity and any planned procedures. Most often its just a wander through the unit and a chat, but if it’s busy I might get to help out for a while, assist with a deteriorating patient, a procedure or tube hold, make a bed, or checks some meds. For me, rounding is an important start to the day as it lets people know I’m here if they need anything, allows me to identify the day’s education plans, and I get a feel for whether I’m likely to be needed clinically for any periods of time.
Once I’ve done this I try to clear my inbox and check my calendar for the day. My day most often has at least one meeting in it, sometimes they start before I’m even at work – I can be directing the children’s breakfast while on a webex. Sometimes I have up to three or four meetings in a day (my least favourite days) and there may be work to review or complete in relation to these either before or after attending.
Many days (my favourite days) are teaching days. This may be at the bedside, or more formally during an inservice period, delivering a presentation somewhere, mandatory training, running a sim or conducting an ALS refresher. Some days I even get to spend the whole day teaching (ALS teaching, or study days for our formal programs).
Most days will throw something unexpected at me, something I can’t plan for and just need to deal with in the moment. This might be a clinical crisis or incident, an equipment issue, it might be facilitating a debrief, meeting with a staff member or product rep for a discussion or even another educator to work through a particular problem.
There is almost always a component of ‘office work’ to my day – what gets done in this time really depends on the most pressing priorities. It might be policy work, it might be working on presentations due for delivery soon, updating ciriculum material, data management, or working on a QI project.
Occasionally (in non COVID times) I get to go out on an excursion somewhere, awards ceremonies, meetings, or external presentations, and if I’m lucky I might get to eat lunch out. I find it impossible to explain to my non-nursing friends just what a treat that is! COVID is occupying a lot of my focus at the moment ensuring good PPE compliance and supervision, and focusing on refreshing skills around COVID intubation, extubation and care of the COVID patient.
What can someone do to prepare themselves for a job as a nurse educator?
Start incorporating education into your nursing role now. Work with students, make time to work with junior staff, take the time to explain things and look things up, role model, participate in policy and procedure review, offer to deliver an inservice and get feedback, apply for backfill in education roles. And get yourself a mentor who can help you.
What clinical concept or topic do you struggle with teaching the most?
It’s the dreaded oxyhaemoglobin curve for sure! I get out the textbook before the lesson and step through it in my head (repeatedly). I get it, but I have always found this concept difficult to articulate to others.
Why is simulation so powerful in education, and how do you use it as a teaching tool?
I am a great lover of simulation and have enjoyed implementing simulated learning into our ICU education curriculum. It’s powerful because we are a practical profession. Many of us learn best by experiential learning. Done well it teaches clinical reasoning, and it comes without risk to patients.
We tend to use in-situ simulation (sim doll, and monitor, set up in a clinical space) and are increasingly doing this in multi-disciplinary sessions for team-based training.
What advice do you have for running a successful simulation training exercise?
My key tips for a successful sim are:
- Plan what you want to get out of the training exercise, and how you’d like it to run
- Have at least one second set of hands to help coordinate and run the scenario
- Allow enough time to set up properly and test any equipment you are using
- Brief people appropriately about what to expect, what the rules are, and how they will be kept safe
- Complete a debrief as part of any simulation
- Evaluate and reflect on how you think it went, and what you’d change for next time.
While I think it’s a great tool, sometimes learners may not be quite so keen. The two things most common comments I get about simulation exercises, especially when people first start to use it are:
- It’s nothing like the real thing…
I have two thoughts about this. Firstly, yes, there are some things simulation just can’t replicate, but in scenario-based sims, the non-technical skills are often more like the real thing than people realise. Secondly, it’s not always important that it’s exactly like the real thing, its about practicing skills, technical and non-technical, so that you use them more intuitively when faced with the real thing, rather than requiring huge amounts of mental energy to think through things analytically in a crisis, or under stress.
- It makes me uncomfortable…
Good! If you’re not at least a little but uncomfortable then you’re probably not learning. What I will do is try to make sure the simulation is a space that is as safe as possible for you to learn within your discomfort.
Post-Grad & Research
You are studying a postgrad in healthcare education – can you tell us about this?
I started a graduate certificate in Health Professional Education (HPE) last year, mainly to obtain an education qualification beyond a certificate IV in workplace training and assessment. For me, it was important to have credibility in the role I hold. I felt I had the critical care specialist qualification and I wanted something in education as well.
I’m doing one subject at a time and will hopefully finish at the end of this year. It’s an inter-professionally based course, so has been very interesting to understand health professional education not just from a nursing perspective but also from medical and allied health perspectives. I’ve done subjects on learning theory and contemporary challenges in eduction, and this semester I’m learning about how to teach clinical reasoning.
What advice do you have for nurses considering postgraduate study? When is the ‘right time’ and how much experience do you think is necessary before undertaking postgraduate study?
I’m not sure there is an ‘exact’ right time for study. It varies from person to person. And just when you think there is a right time, the kids have started school and you have the brain space, a once in 100 year pandemic happens. Your kids are suddenly supposed to be home-schooled and your second assessment asks you to keep a log of all teaching activities for a period of time when your workplace tells you all teaching is to be cancelled! But I’m not easily put off when I make a commitment to something…
I think you fit study in when you can, when you have the mental energy to get out of it what you want to get out of it and when you deem it to be a priority at a particular point in your life. I do advise my transition staff not to undertake separate postgraduate study while completing their transition to critical care program. I want them to focus on the learning from the program, and since we’ve had this program accredited with two units of a Post Grad in Critical Care, they are effectively already doing part of their post grad by completing the program.
When staff complete transition, some undertake a period of consolidation, some move straight into post grad study. I support both of these approaches but do like to see our permanent staff, who wish to remain in ICU long term, undertake a PG at some point during their early career so that we stay in line with maintaining a 50-75% specialist qualified staff as recommended by the ACCCN.
What areas of research are you interested/involved in?
Other than regular survey participation, I haven’t really been involved in research on a large scale. People keep asking me if a PhD is in my future… honestly I’m not sure my husband would survive me undertaking more study, but I haven’t ruled it out somewhere in the future.
On a smaller scale, from a quality improvement perspective, I had been involved in a few different projects:
- As part of my masters I undertook some auditing looking at oxygenation practices in ventilated patients in the ICU and used that to develop hyperoxia education for staff and a hospital protocol on oxygen therapy.
- In 2017 I was a successful applicant for a professional development scholarship through SYNERGY (The Research Centre for Nursing and Midwifery), which looked at attitudes, beliefs and practices related to sedation in our ICU. This led to education for staff and a further QI that implemented a delirium screening tool.
- Last year I led a group of staff to rollout a QI project involving pre-packaged mouthcare products to improve nurses understanding and compliance with mouthcare in ventilated patients.
I read endless amounts of research as an educator and have lots of interest areas – anything related to critical care, resuscitation and/or education is of interest to me.
What keeps you busy when you’re not working? And how do you find a healthy work/life balance?
I enjoy spending time with my husband and two kids. We like to go camping as regularly as we can and usually try to plan at least one holiday per year with our camper trailer. We have been fortunate enough to set up camp in many great places within Australia including the iconic Uluru and West Macs, Kakadu, the Warrumbungles, the Flinder’s Ranges and out across the Birdsville Track. There’s something quite restful about a campfire. I love the desert (it may have something to do with lack of phone service and wifi – I’m uncontactable and cannot access my emails!). Aside from camping I love reading and enjoy a good baking session.
Honestly, I’m not sure I always achieve a healthy work life balance! But it is something I am working actively on. This year I am setting better boundaries, as well as alarms on my phone (the ‘Go Home Now’ alarm is helping me to leave on time). I have set ‘wind down’ time and ‘sleep time’ on my phone so I am getting better at getting a good night’s sleep. And I am trying (and not always succeeding) to do more exercise.
What are your future plans or career goals, and where do you see yourself in the future?
Short term I will complete my certificate in health professional education and continue to take opportunities to build myself as an educator. Being an ICU educator was my dream job when I started out – still is if I’m honest about it, I love what I do. Medium term I’m planning how I can use my long service leave to take a few months to travel the top end of Western Australia. This has made me think about succession planning for my role, even if it’s just short term. Long term, maybe one day I’ll make it into the tertiary education sector or get to the PhD…
Imposter Syndrome
I’ve learned that imposter syndrome is a real thing. You feel it as you enter the workforce (I don’t know enough), you feel it as you move up the ranks (I haven’t got the experience for this), you feel it in the education space (I shouldn’t be doing this job as I don’t have all the answers).
But there are three things I have learned:
- Always be working to build the skills you want to have because if you wait until you are ‘ready’ to do something, you will never actually do it. You’re never 100% ready so make the most of opportunities as they arise!
- Experience, and reflection on that experience, is the best teacher in the clinical environment, and as long as you maintain the capacity and openness for learning you can move forward.
- Good educators don’t give people all the answers, they guide people to develop the knowledge and skills to find answers for themselves.
What is your leadership style?
Styles of leadership can be dependant on a particular situation. For example, when I look at Goleman’s six styles of leadership, I can think of an example of how I might use each, depending on the nature of a particular situation. When dealing with a novice learner in an emergency situation, I might use commanding leadership. If I was dealing with a learner acquiring a new skill I would be more inclined to use coaching. But if I am dealing with our senior-level 2 nurses in a discussion about change I would be more likely to use a combination of democratic, visionary and affiliative approaches.
Overall, and in line with my values, I am drawn to the qualities embodied by that of transformational leadership and authentic leadership. Stanley (2011) describes the four essential themes in transformative leadership as clear vision, communication of that vision in a way that inspires and empowers others, consistency and authenticity that builds trust, and self knowledge or emotional intelligence. Authentic leadership is about functioning in accordance with your values and beliefs, and your credibility is built on your actions resonating with what you say.
I have a clear vision for what I want education in our department (and healthcare in general, if I’m honest) to look like. I believe in and try very hard to practice transparent communication. While reactionary measures are sometimes required in healthcare, I’d rather prevent something by putting in place structured education or support systems and by being approachable and open to change, rather than deal with the consequences when something adverse happens. I believe in the importance of role modelling – if people see their clinical leaders doing something, they are more likely to do it themselves: good or bad. I would also not ask something of someone I am not prepared to do myself.
Who are the people who have been most influential to you and why?
I tend to think about this in terms of personal influences and professional influences. Personally, my parents have been a huge influence on my work ethic and belief that I could do whatever I set my mind to. I was very close to both my grandmothers, who taught me the value of family and how to build resilience. My husband is a huge influence, as are my children (who have taught me more about myself in the last 7 years than I knew in 30 years before that!).
Professionally I think there are three key people who have influenced me – one in the clinical sphere, who taught me the value of holism and inspired my interest in end of life care; one in the education sphere, who gave me opportunities to grow myself; and one in the leadership space, someone who taught me about strategy, about advocacy for patients, but also advocacy for your staff, and why trust and transparency are so important.
You are involved with the ACCCN, what does this entail?
The Australian College of Critical Care Nurses is the organisation that supports and advocates for our specialist critical care nurses. They do important work in lobbying for safe workforce ratios and supports within critical care, represent the critical care nurses’ voice within other peak committees and organisations, contribute to improved care and outcomes for the critically ill patient, support critical care research and evidence-based practice, and provide education opportunities and leadership relevant to critical care.
Their aims align with many of my professional values and that unpinned my membership with the organisation initially, and then my decision to become more involved with the college. I’ve had some amazing opportunities as a result of my involvement, such as working on the development of the position statement on critical care education; sitting on event organising committees, and joining the ACT/NSW branch committee. Perhaps the most recent has been the opportunity to co-convene the ACCCN’s annual education meeting held in Canberra in May this year. Additionally, I also get to work with some really fantastic people, who taught me how to use video-conferencing long before COVID made it the done thing!
Can you think of a really funny situation you’ve had while working?
Oh maybe the time a 95-year-old man asked me to fetch his boxer shorts that had the catchphrase ‘always got time for a quickie’ printed on them. Still makes me laugh when I think of it.
I can think of a lot of funny situations, many of which are inappropriate to share in this forum. Sorry! Like many nurses, especially critical care nurses, much of my humour can be on the dark side and that gets reserved for the inner sanctum of people who know me well enough to know that if we didn’t laugh about some things, we’d spend an awfully long time crying…
If you were invited to do a TED talk, what would be the title?
I’m really bad at titles. What about ‘Nursing education: what’s in it for me?’
Read part 2 of Rachel’s interview HERE!




You must be logged in to post a comment.