Table of Contents
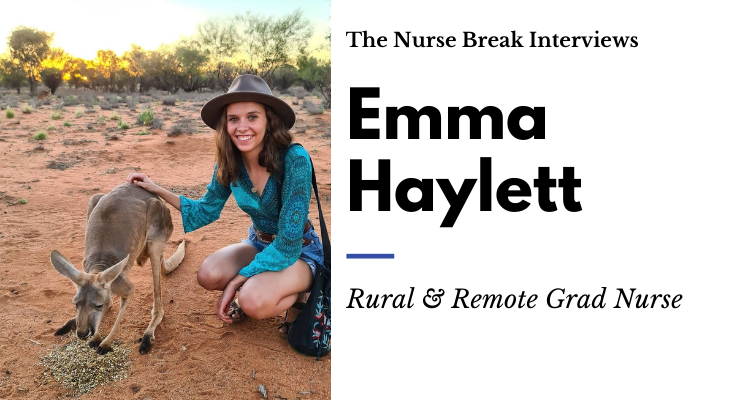
Hi, my name is Emma Haylett and I am a 2020 graduate nurse from tropical North Queensland who has found myself crossing borders to the Middle of Australia in the midst of a pandemic to complete her graduate nurse year in Alice Springs. Yep, if you thought a graduate year was already stressful enough, try again!
Join our new FB group Rural & Remote Nursing | The Australian Outback
Emma has also written about her nursing placement and student experience HERE
Keen to go RURAL & REMOTE as a Grad or later in your career? This Q&A will EXCITE you!
Quick dip at Redbank Gorge after a night of camping Visiting Uluru with some nurse friends New Graduates – Genet, me and Dharanish finishing up on Surgical ward

What was your graduate application process like?
The graduate application process is nerve-wracking and confusing but my biggest tip is to challenge yourself and give yourself the most opportunities by applying far and wide! I was offered 3 positions in total and I also knocked back an interview for the Cape York region due to already accepting the Alice Springs offer. By only applying for one hospital and one specific area you are limiting yourself and giving yourself less of a chance in obtaining a graduate position. Still apply for that area but also apply rurally, remotely, in other states etc to give yourself more opportunities.
I also recommend that towards the end of your 2nd year and into your 3rd year making sure you always get contact details for referees and feedback where you can ready for the application process. Making yourself known to the Nursing Unit Manager of the ward you want to work in can also help as they will be able to put a face to your name. If you’re lucky enough to get an interview, make sure you know the values and mission statement of the Hospital you are applying for and know how you can meet those values with personal examples as you want to sell yourself as the best candidate for that particular hospital/ward.
Whereabouts is your grad year?
Smack bang in the middle of Australia, completing my graduate year in Mpartwe (Aboriginal word for Alice Springs). I have almost finished my 12 months graduate year in the Alice Springs Hospital.

What is the size of your hospital?
Surprisingly for a town of roughly 25, 000, the hospital is quite big with 180 beds that encompass 2 medical wards, a rehab ward, a surgical ward, palliative care ward, renal ward, dialysis ward, intensive care unit, emergency department, mental health ward, paediatrics and a maternity ward. This number however doesn’t take into consideration the catchment area of 1.6 million square kilometres it services which stretch across bordering remote communities in WA and SA!
What type of staff ratios, rosters and shifts do you have?
On the Surgical Ward, we had ratios of 5 patients on the morning shift, 6 on the late shift and 8 on the night shift. I think this is the same ratio for most of the wards in Alice. In the ED it varies on the area you are in, in the acute areas I find myself having 3-4 patients and in other areas of higher dependency you might have 1-2. The new graduate program out here in Alice is a full-time position (with the ability to drop to .8 if necessary). We work 8-hour day shifts and 10-hour night shifts in most wards, although I believe ICU do have 12-hour shifts.
What clinical services exist?
In Alice Springs Hospital we are fortunate enough to have a wide range of professionals working beside us. There is a big intern program, physiotherapists, occupational therapists, dieticians, diabetes educators, wound care nurses, pharmacists and personal care assistants whom all help to deliver a high standard of patient-centred care with good clinical outcomes. A lot of our patients do come via RFDS transfer to and from the hospital so there is some liaisoning and paperwork to prepare at times before transfers but the majority of the times things go smoothly.
Did you feel supported?
As a graduate, I have felt very well supported throughout my program at Alice Springs Hospital. Graduate educators are present that follow you throughout the year, check up on you and are also available if you need assistance with anything. On top of this, each ward has a clinical educator and senior staff that are also available for any questions or concerns. I have never felt stuck or alone and have always had someone to turn to in scenarios where I felt unsure.
Camping trip to Rainbow Valley with great mates A painting I bought from Santa Teresa artist, Sheree Doolan. Great artists often come to sell paintings to healthcare staff at the hospital Christmas day shift swap
I have met some amazing nurses and allied health staff who have made the Alice Springs journey so special. I really believe you meet some of the best people working out here in Alice Springs and everyone gets along so well – it is unlike any other hospital in terms of the friendships that are built.
What was your graduate program structure like?
The graduate program allows graduates to put down preferences in three areas they would like to work. The graduate coordinators do their best to try and give everyone a placement in at least one of their preferred areas. The program goes for 12 months and the graduate nurse gets two rotations each of 6 months in length.
What were your rotations like?
I have done 6 months in the Surgical ward and have almost completed 6 months in the Emergency Department. The biggest challenge for both areas was getting used to time management and the different priorities for different areas. In surgical at first, I was trying to get my head wrapped around the different observations needed for post-op patients, the making up and use of patient-controlled analgesia, the medications that should be withheld pre-operation and the different types of dressings used for different wounds.
The great thing about having started in the Surgical ward is that it developed my time management skills quickly and has left me with knowledge on wound dressings that I may not have got in other areas. I realised this when I was asked to do some dressing in the Emergency Department and was asked my opinion on what would be most appropriate to use by a doctor. I realised that I had this knowledge locked away and saved in my brain from my time in the Surgical Ward.
Moving to the Emergency Department was a completely different ball game and suddenly I couldn’t plan out my day using planners anymore – crossing tasks out as I did them. The thing about the Emergency Department is that patient flow means patients are moving through the different areas of ED and then eventually being discharged home after investigation or moved upstairs to a ward for further care. This makes it impossible to plan for the day as patients are coming and going frequently and investigations and tasks vary depending on patient to patient.
I found it challenging at first to get my head around the paperwork and dynamics of the Emergency Department but have learnt to love it. Both areas have greatly improved my time management skills in different ways. The positives of ED are being a bit more independent in assessment and investigations and also seeing and being exposed to lots of different hospital presentations.
Accomodation?
As a graduate nurse, you are offered a room in the hospital quarters ($140/week which comes straight out of your paycheck). There are two buildings – Stafford and Denison with 3 floors to each. The quarter’s rooms are quite small but have a desk, cupboard, king single bed, bedside table and a sink in them.
Each floor has two shared kitchens and one bathroom with five showers and toilets. The quarters are a great way to meet people and socialise especially when new to town. I lived in the quarters for 10 months before finding a share house with some girls I knew from work. People tend to do this and stay in the quarters until they have met some people to move out with. The maximum time you can spend in the quarters is 12 months before you must find your own accommodation outside of the hospital.
One of the shared kitchens At least it has a sink My room on arrival…. Dorm room on leaving… just needed some fairy lights and plants!
Social Activites?
We get up to a lot! If you love outdoor activities then you will love Alice Springs. We often have big camping trips as well as day trips out to waterholes. If you don’t own any camping gear now, you will after a few months in Alice Springs and you will own a swag by the end of your stay. We often cook our food over the campfire with the camp ovens and grills and get up to some 4×4 driving as well on these little adventures. We also tend to a lot of hiking around the place with some amazing views. There is so much to see and do out here!

Other than camping there is also trivia on Thursdays at Montes, Karaoke at Uncles on Fridays and live music on Tuesdays and Thursdays at some of the local bars. There is always something exciting and fun to do and plenty of people around to hang out with. We also have some really fun festivals out here like Parrtjima (Indigenous light festival), Fab Alice, Beanie Festival, Film Festivals, Wide Open Spaces, Camel Cup, Todd River Regatta and Finke Desert Racing. There’s always something fun happening around the place.

What types of patients did you look after and what makes remote nursing unique?
In Alice Springs Hospital we have a large Aboriginal population who mostly come from out in community or town camps. This can pose some language barriers as some patients from out bush can’t speak a lot of English. We are lucky in Alice Springs Hospital as we have Aboriginal Liason Officers from each language group encompassed in the catchment area to translate where needed.
The ALO’s can assist in a range of tasks but mostly translating patient concerns to health staff as well as translating the importance of a health conversation/message to the patient, such as gaining consent for an operation. Unfortunately, many Aboriginal patients have co-morbidities such as type 2 diabetes, rheumatic heart disease and renal failure. As a result, there are many presentations to the ED with missed dialysis.
It is also not uncommon for patients to receive LA Bicillin on a hospital admission due to rheumatic fever cases and rheumatic heart disease (and if you have never given it before- it is not pleasant!). The western model of healthcare can at times clash with the holistic healthcare approach of Aboriginal patients with their lifestyle and cultural commitments. For example, Sorry Business is very important to Aboriginal patients and is often a reason for a patient to leave the hospital or miss dialysis.
Have you done any upskilling during your graduate year?
Since being here I have done my Venepuncture and Cannulation course through the hospital and have also done my Understanding Vaccines and the National Immunisation Schedule course online. I hope to do some ALS training this year at some point.
The things you wish you’d known before you started?
I wish I knew how cold it got in winter! Down to 0 degrees – this North Queensland girl was not prepared for that. I now I own some Kathmandu thermals and a down jacket for the first time ever!
What’s next for your career?
I have applied to continue working in the Emergency Department in Alice Springs and am waiting to hear back about my application. I hope to stay in the Emergency Department and would like to do a rural and remote postgraduate certificate in the near future. My aim is to do rural agency work once I have accumulated more experience as a nurse.
Where can people find you online?
I am always open to questions, especially from people who are interested in going rural and remote. You can see more of my pictures, asks questions and follow my journey on Instagram @emmajaneeh
Emma has also written about her nursing placement and student experience HERE















You must be logged in to post a comment.