Table of Contents
Dr Karen Hammad has held positions in the university sector, as a hospital coordinator and as a health care consultant for international organisations such as the World Health Organisation and private business. Karen graduated as a Registered Nurse in 1996 and has continued to work in a clinical capacity since this time in public and private emergency departments in South Australia. She holds a PhD, is a business owner and passionate about disaster preparedness and nursing!

She currently works as the Clinical Management and Infection Prevention and Control (IPC) Pillar Lead in the Incident Management Team (IMT) for the World Health Organization (WHO) in Papua New Guinea (PNG).
During 2020 before moving to PNG she worked with WHO Euro region in the Copenhagen Incident Management Support Team (IMST) course and to support the COVID-19 response in Europe by assessing hospital readiness and providing technical support. In 2019, she worked for WHO Headquarters in Geneva on health security predominately related to chemical and biological readiness.
Tell us about your journey into nursing?
I didn’t want to become a nurse actually. As soon as I finished high school I moved to Scotland for a gap year. My parents completed the university entry forms for nursing and I will never forget the day they rang and told me I got into nursing. I told them I wanted to stay in Scotland and travel the world. That response didn’t go down well with my parents and they somehow convinced me to come back to Australia and complete a nursing degree, after which I could do whatever I wanted to do. I reasoned I could probably use my degree to travel the world doing humanitarian work and I clung to that hope.
I didn’t enjoy studying nursing and I am amazed I passed my degree. When I graduated I did a graduate nurse program in 1996 spending 6 months on the renal ward and 6 months on the orthopaedics ward. After that, my mind was more or less made up to quit nursing. Not to diminish the amazing work that ward nurses do in any way, I just felt like it wasn’t for me and as that was all I knew of nursing, I felt convinced also that nursing wasn’t for me.
The emergency department, however, looked quite interesting when I had passed by. I had never worked in the ED or done any student placements there but I went down and had a chat with the nurse manager to see if I could try working there. She said she could give me a 3-month probationary contract. Her willingness to do this changed the course of my life because if she hadn’t have given me a chance I would have quit nursing. I fell in love with emergency nursing from my first day and the 3-month contract became permanent.
What do you love about nursing?
I love the diversity of the nursing profession. Nurses can specialise in different areas and work in many environments. Our nursing skills are also transferrable making us highly employable in other settings. I would recommend a career in nursing because nurses can quite literally make a difference. Nurses greatly influence how an individual experiences their interaction with the health system and a good nurse will make the experience less painful, less challenging, less scary and less lonely.
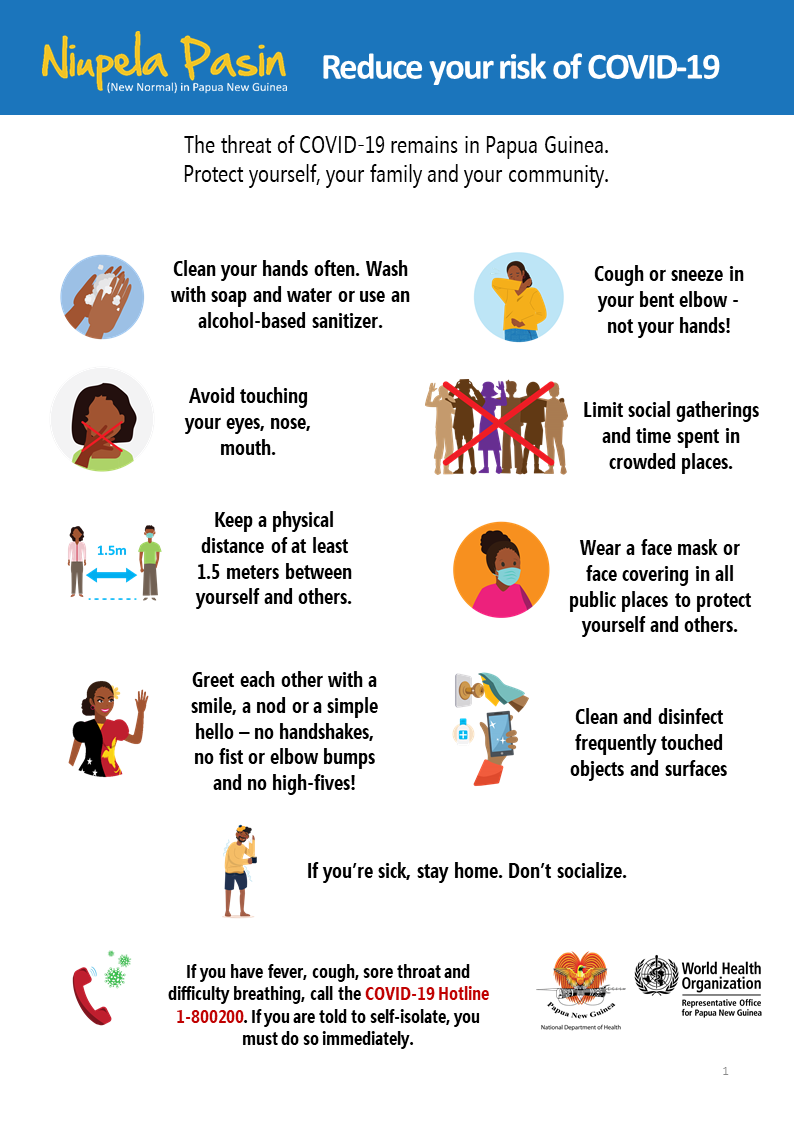
Nurses are well trusted in the community so they can also make a difference through educating the public and role modelling good health behaviours. There has never been a more important time to do this than during the COVID pandemic where non-pharmaceutical interventions such as mask-wearing and physical distancing are important measures to slow transmission.
World Health Organisation

What is your involvement with the World Health Organisation?
Currently, I am working as the Clinical Management and Infection Prevention and Control (IPC) Pillar Lead in the Incident Management Team (IMT) for the World Health Organization (WHO) in Papua New Guinea (PNG). The Incident Management Team is the in-country team responsible for managing and implementing the WHO response to the emergency. I work closely with other WHO consultants, the National Department of Health and other partners from UN agencies and non-government organisations in the COVID-19 response in PNG.
During 2020 before moving to PNG I worked with WHO EURO in the Copenhagen office where I helped to design and build an Incident Management Support Team (IMST) course and to support the COVID-19 response in Europe by assessing hospital readiness and providing technical support. In 2019 I worked for WHO Headquarters in the Geneva office where I worked on health security predominately related to chemical and biological readiness.
What does a typical day in this role entail for you?
There is no typical day for me. When I am at my ‘home base’ in Port Moresby I work closely with the WHO IMT and National Department of Health (NDOH) colleagues in the National Control Centre (NCC). Our focus is to ensure an effective response to COVID-19 in PNG. Throughout my days I might be attending various meetings, working on clinical management or IPC strategies and guidelines, delivering training for health staff or visiting health facilities in the area to see how they are managing COVID-19 and providing technical support if needed.
When I am on duty travel out to the Provinces I am largely undertaking activities to support the local health authorities to manage COVID-19 such as assessing health facility readiness, building health system capacity, providing training for health workers on clinical management or IPC topics and supporting the IMT to manage an outbreak situation.
The work I do is very much as part of a team, the IMT, the NCC team, the team that travels out to the Provinces to provide support, or the team in the Province. None of this work can be done alone. So, if I develop a document or guideline there is a team of people whom I have collaborated with. If I visit a Province, I go as part of a multidisciplinary team. When I am in the Province I work with a team of health workers to implement strategies.

Why are the number of COVID-19 cases and reported deaths currently low in PNG?
It is hard to comment on why COVID-19 deaths are low in PNG and why we have not seen the severity of cases that they have had in other countries. Most of our cases have been mild or symptomatic and it seems that COVID-19 is not so bad, making it hard to see why we should keep going with the response and with Niupela Pasin. The truth is COVID-19 is still a new virus and we don’t know enough about it yet; we don’t know what will happen in PNG if the virus mutates or if different strains enter the country. This is why we need to remain vigilant so that we can protect the people of PNG.
Why is Niupela Pasin / the new normal so important?
The only way we will be able to stop COVID-19 is if we all adopt Niupela Pasin. Washing hands, wearing masks and physical distancing are the most effective ways to stop the virus from spreading at the moment. Health workers can’t fight this alone, this is everyone’s fight. Actually, this new normal is effective at slowing the spread of many other infectious diseases so the benefits are not just for COVID-19. Of course, these things seem hard for us now because we are not used to doing them but if you really think about it, washing or sanitising your hands regularly, wearing a mask or physically distancing from other people are small things that you can do to help fight COVID-19 and help protect your Wantok from getting sick or even worse, dying. We are all in this together and we all need to work together as one big wantok to fight COVID-19 and protect Papua New Guinea. If everyone commits to this, we can enjoy a life without lockdowns and travel restrictions.
What has been your highlight in PNG so far?
There is so much that I have enjoyed about PNG so it is hard to pick one moment or one thing as a highlight. I have been very lucky to visit some of the Provinces and see for myself the natural beauty of PNG, meet the locals and eat the fresh produce from the roadside market stalls. As a nurse myself, I think the highlight of my job in PNG is meeting and working with so many inspiring nurses, doctors and health workers in the hospitals, clinics and aid post who work hard and remain resilient providing the best care they can even when they don’t have the basic things they need such as running water or consistent power supply. I feel truly privileged to have the opportunity to work here.
What are some of the unique challenges and rewarding aspects of your role within the World Health organisation?
One of the biggest challenges of this role is that there is no ‘one size fits all’ approach. Just because it works in Australia for example or an international guideline says it should happen a certain way, it doesn’t necessarily mean it will. Differences in culture, language, politics, finances and existing health practices mean that you need to be patient and find different strategies and think outside of the box a lot of the time.
This is one of the most rewarding roles of my work life, and it’s not just because my work is directly related to a historic pandemic that will be in living memory for a long time to come. In my role, I can contribute to a national pandemic response through the development of guidelines and policies that direct COVID-19 management. I can help build health system capacity where it is really needed.
Most of all I have also been able to work closely with the people of PNG and in particular the health workers whom I admire so much for their resilience and the amazing work they do in incredibly low resourced settings. So although I am not actually nursing patients, I am working as a nurse in the humanitarian field, so my work dreams have finally come true.
How would you best encourage nurses that are interested in international and volunteer nursing?
I would recommend doing it. Working in urban health settings in Australia you really have no idea how privileged and well resourced we are until you visit health settings in other countries where basic amenities like running water and a constant power source are lacking. You get to work with many amazing and inspiring individuals who are all working for a common goal.
You get out of your comfort zone, you get to travel this amazing world and have so many amazing experiences that you never would have had if you stayed at home working in the same hospital for your entire career. Most of all, you get to meet real people who live lives so different from you, beautiful people who are grateful for the work you are doing to support them and help their country.
Disaster Preparedness and Nursing
Where did your interest and passion for disaster relief and management come from?
9/11 was a defining moment for me. Not because I was there, but because I watched, with many other people around the world as the disaster unfolded before our eyes on television. Before 9/11 I had only seen the aftermath of natural disasters such as bushfires, earthquakes, floods and famine, but 9/11 dominated the media and I stayed up half the night watching television. My thoughts quickly went to the ED staff in New York and what they must be going through.
Then I started thinking about what would happen if something like that happened in our city. At the time I hadn’t worked in any disaster situations, I hadn’t done any disaster training and I didn’t even know such a thing as a disaster plan existed. Here I was 6 years into my career having a realisation that when disasters happen emergency nurses are on the frontline because I am watching it on television.
It shocked and disappointed me that disaster response was absent from our university degree, and from the orientations or professional development at any of the hospitals I had worked in, to that point. I wanted to learn all that I could to prepare myself. As I spoke to other colleagues I discovered they also felt unprepared and lacking in knowledge about disasters and so my passion to prepare and build resilience in health workers grew.
What is your company ‘Disaster Readiness Solution’?
I started Disaster Readiness Solutions to continue my passion to build a community that is aware of the impacts, prepared to respond and resilient to disasters and unplanned events. We provide training options and consultancy services to health care organisations, health workers, small business, local council, community groups and schools as well as easy to access online training options for individuals.
Our consultants are disaster experts with strong experience in disaster preparedness activities (including simulation, training and planning), research, education development and design, policy and procedure writing and facility preparedness.
Assessing a health facility for diaster readiness basically requires me to get an understanding of what processes and systems are in place as well as what preparedness activities have already occurred. I enjoy assessing readiness because I can provide tangible solutions to improving readiness.
What are some of a nurse’s role in disaster relief response and management?
Nurses play a vital role across the disaster continuum from preparedness and planning to response and recovery. Nurses should provide a voice on their health facility disaster planning committee and contribute to preparedness activities to ensure that the health facility is ready to respond. Nurses should be aware of the hazards in the region and the likely impacts of those hazards requiring a health response.
Nurses need to know what their role is in disaster response and should know what the facility plan is. Nurses, as the largest health workforce group are vital to disaster response, particularly in front line roles. Nurses in management positions should be responsible for ensuring staff are aware of the disaster plan and have training opportunities to prepare them for disaster response. Nurses in the disaster-affected community will play an important role in the recovery process supporting people who are displaced or injured and addressing the mental health effects of the disaster.
Disaster relief education?
I have worked for 10 years in the university sector where I developed a Masters Degree in disaster health. The degree was for allied health staff (such as nurses, doctors and paramedics) and provided them with a tertiary qualification. At the time it was one of the first tertiary courses in Australia that focused largely on the operational response to disasters. I strongly feel that as a topic, disasters preparedness, response and recovery should be discussed in all undergraduate nursing, medical and paramedic.
The topic should also be discussed in postgraduate nursing studies for specialisations who work in frontline roles such as emergency nursing and critical care nursing. Additionally, for those who want to pursue a career in emergency management or who would like to be part of humanitarian response, I would like to see non-government organisations and universities collaborate on specialised post-graduate programs to prepare health professionals for disaster response. Currently, there are limited opportunities for nurses to pursue postgraduate disaster studies in Australia.
COVID 19 pandemic impact
The COVID-19 pandemic has increased the demand for nurses full stop. Nurses working in clinical roles in regions where the pandemic has overwhelmed the health system have been overwhelmed. We have also unfortunately seen many nurses infected by COVID-19 and have lost many colleagues around the world to the pandemic. COVID-19 has heightened awareness of pandemics and the role of nurses on the frontline response to such events.
Leadership & Research roles
You’ve also held the role of a hospital coordinator. What does this involve?
A nursing hospital coordinator is basically someone who oversees the hospital operations largely from a nursing perspective. It is busy and feels a lot like you are putting out spot fires. Some of the things I would do would be to ensure we had adequate staffing levels, ensure sick leave is covered, support any staff who are injured or become unwell at work, oversee patient flow through the hospital to ensure there were no long delays, facilitate transfers to other hospitals, act as disaster controller if the general manager is not present, present to any hospital codes and manage customer relations issues.
To become a hospital coordinator you would have to be a very experienced nurse with a very good understanding of the hospital you are working in. There is no specific pathway for becoming a hospital coordinator, but desirable qualities are someone who demonstrates leadership, calm under pressure and can have a global view of hospital operations.
Challenging aspects of the role?
The most difficult part of the role I find is that usually, everyone wants you at once. While you are trying to manage sick leave for the next shift, the staff in theatre might be calling to say that the ward staff are too slow to pick up their patients, another hospital might be calling to request a transfer of a patient, the code blue alarm goes off and then someone on the ward had a needle stick injury. All this action is interspersed with moments in the office doing administrative tasks.
Things nurses on the floor may not realise about the role?
I think nurses on the floor see someone wandering into the department or ward with a clipboard looking officious and asking questions about staffing, it looks like an easy job when they are run off their feet answering call bells and giving out medications. Often people are often only aware of their bubble and might not see beyond this to understand all the things that are happening concurrently throughout the hospital that the hospital coordinator might need to respond to. As a clinician at heart, I am more than happy to answer a patient bell when I walk past and grab a bedpan as I walk past the sluice room. But if I get too bogged down in helping then I might not make it to a code in time.
How would you best encourage junior nurses to take on leadership and management roles?
I think all nurses need to show leadership in their roles when they advocate for their patients or when they are providing opportunistic health messages to their patients. I would like to see more junior nurses have the opportunity to take on management roles or be mentored into leadership positions. Too often in my nursing career, I have seen people who are ill-equipped as leaders get into management positions and stay there.
The worst managers I have come across are those who have had limited experience outside the organisation and stay in their management role for 20 plus years. This stagnates the department or organisation as a whole and prevents younger staff or people who have had a wide array of experience outside of the organisation from getting into management positions and bringing with them new and interesting ideas. If I could change anything about nursing it would be this detrimental practice.
Outside of nursing, I would like to see more nurses take on leadership roles in other areas such as politics and organisational boards. Nurses have a wealth of knowledge and can have a strong voice influencing public policy and agendas aimed at keeping our community safe and building better health systems.
You have also done a PhD in nursing. What is nursing research all about?
I didn’t plan to do a PhD but my passion for preparing nurses for disaster response drove me to it. I remember feeling completely unprepared for disaster response and knew through conversations that many of my colleagues did also. So I did a small study to understand the disaster education and training of emergency nurses in South Australia.
When I presented the study at the World Congress for Disaster and Emergency Medicine in Amsterdam in 2007 I met my future PhD supervisor who was presenting at the conference. He suggested I do a PhD. This was a crazy idea, I was a clinician and I saw nothing beyond me at that stage than working in the ED for the rest of my career.
He somehow convinced me to do an Honours Degree which was followed by a PhD. My PhD was about the experiences of emergency nurses in different countries who had responded to a disaster while working in the ED. It took me 5 years to do my PhD while working full time as an academic at a University. My PhD coincided with a few challenging experiences in my personal life and it was a big commitment and a difficult journey.
What kept me going personally, was my passion for preparing nurses for disaster response. Finishing my PhD has been one of my biggest life achievements and something the young Karen who got very average grades at highschool never would have anticipated getting.
I would recommend to anyone interested in undertaking a PhD to focus on something they are passionate about. A PhD is a long journey so you need a topic that will maintain your interest and attention for a number of years. For similar reasons, I would recommend choosing a supervisory team wisely. You will have to work with these people for a number of years.
Final Questions
If you were in charge of nursing for Australia, what would you do or change?
If I was in charge of nursing in Australia I would of course ensure our tertiary programs had more disaster content. I would also ensure it was mandatory for all health facilities to do regular disaster drills and staff training to prepare them for disaster response.
What advice would you give your younger nurse self?
Nursing is not a glamorous job but it is rewarding and you can have an exciting path ahead of you if you step outside of your comfort zone and take up opportunities that come your way. The heart of nursing will always be providing patient care.
What is the key to a successful nursing career?
The key to a successful nursing career is recognising that nursing is not just a job it is a profession. Someone whom I believe has had a successful nursing career has a solid foundation working as a clinician for a number of years and has either progressed to a senior role in the clinical area or who has used their clinical nursing experience as a foundation to give back to the nursing profession or work towards the betterment of health provision for the community.
Enjoyed this article? Check out the others HERE








You must be logged in to post a comment.