Table of Contents
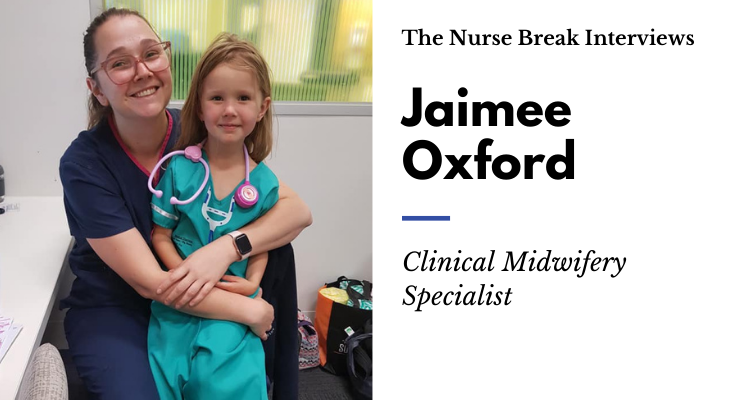
Meet Clinical Midwifery Specialist Jaimee Oxford. She shares with you in this Q&A what a Clinical Midwifery Specialist is all about!

Tell us about yourself?
I’m a Clinical Midwifery Specialist working in a large Hospital in Regional Victoria. I have recently returned to volunteering for St John Ambulance after a hiatus whilst focussing on other projects. Outside of work, I am a single parent to a gorgeous 6-year-old who generally keeps me pretty busy.
I have always known that I wanted a career in healthcare as my dad is a Paramedic and St John Ambulance volunteer. Growing up in the Northern Territory meant that my siblings and I grew up helping our dad if he came across trauma. Whilst I initially planned for a career as a doctor, a former partner was studying nursing which sounded interesting, and I decided to switch from Biomedical Science to Nursing and never looked back.
Can you tell us about the early years of your career, before becoming a Midwife?
Whilst studying nursing, I continued volunteering for St John Ambulance and I loved working in their field hospital at large events so my plan for my nursing career was to work in the Emergency Department. I graduated from nursing in 2011 and completed my graduate nursing year in a Regional Victorian Hospital. One of my rotations was three months in a rural Hospital which had an Urgent Care centre.
I loved this opportunity to consolidate my skills and learned a lot about managing deteriorating patients until they could be transferred out to a larger hospital. After my graduate year, I began a Specialist Transition Year which involved me rotating between ICU and ED. This sparked my interest in ICU Nursing as I loved the intricacies involved. I had planned to complete my postgraduate diploma in Critical Care, however, I moved to a larger Regional town as my former partner was transferred for their employment. After that move, I worked in Aged Care for a brief period until I went on maternity leave.
Where do you currently work and what inspired you to work in this field?
I currently work in a large regional hospital as a midwife and nurse. When I returned from maternity leave, I worked casually in ED, ICU and Medical Imaging as a permanent job was hard to find at this hospital at that time. It was during my pregnancy that I started to think I might want to study midwifery. I was lucky enough to receive care during my pregnancy, labour, birth and beyond from two wonderful midwives who inspired me to think of midwifery as the career for me.
I was employed as a student midwife by this hospital and over 12 months I was supported to complete my studies whilst working on the maternity ward. During my pregnancy, I loved the rapport and relationship that midwives were able to develop with their clients. I loved that they had such an impact on my parenting journey, and I wanted to be able to do that for others.
Can you tell us what your role involves as a Clinical Midwifery Specialist?
My role involves supporting and mentoring my midwifery colleagues in the areas that I work in which are Women’s Ward, Birth Suite, and Women’s Clinic’s. I also offer support to student nurses and midwives and doctors when on placement at our hospital. I also often work in an Acting ANUM capacity, which means I work as the midwife in charge of either Birth Suite or Women’s Ward depending on where I have been allocated that day. If I am working in the Birth Suite then I need to try and attend each birth so that I can be there to support other staff.
I also would have an overall view of what is happening in the area that I’m managing, conduct ward rounds with the medical team, and I’m there to support both midwifery and medical colleagues throughout the shift. Whilst women are in labour we will regularly attend each room, to check in with the midwife caring for the client, look at any monitoring that they may be having and have an understanding of what stage of labour the client is in and if any additional support is required.
To be a CMS, you must work on some form of Quality Improvement project or Clinical Standard, and I have worked on several over the last 4 years. All midwives are also required to annually complete Neonatal Resuscitation, Foetal Surveillance Education Program (a certain score is required depending on your qualification), we also complete a study day of Simulated Obstetric Emergencies, this is on top of our professional development requirements as nurses.
The world of midwifery can bring so many amazing things. I always feel so privileged as I get to be present for such a life-changing moment. We are advocates for our clients and we always want to support them. Midwifery is so much more than people picture as we are present for so many different moments in a person’s life. We care for clients who may have experienced trauma and try to find a way to make them feel safe and supported.
Being a midwife is a privilege as we are able to connect with our clients in so many different ways. I can see clients years down the track who remember that I was present at their birth or was there for them during a challenging time, and I feel so lucky to have been able to be there.
What are the main types of patients you see as a Clinical Midwifery Specialist?
I see patients at every stage of their pregnancy as I work in several areas. I work in Women’s Clinic which means I see clients who are early in their pregnancy (generally 16-17 weeks at our hospital) and will do a comprehensive assessment to collect their past medical history, family history and obstetric history. This helps us to identify whether the client requires low-risk midwifery care or high-risk Obstetric care. I also see clients throughout their pregnancy and will check their blood pressure, symphysis fundal height, foetal heart rate, and will arrange any pathology or radiology that they need at that stage of pregnancy and if necessary escalate care to an Obstetrician.
We provide education on pregnancy, labour, breastfeeding, discuss common discomforts of pregnancy, and will educate clients on common discomforts of pregnancy as well as when to come to the hospital. A lot of the work done at this stage is about building rapport so that we can all support our clients through their pregnancy. This can involve trying to support clients to quit smoking or illicit substances or reduce their intake. We are a multi-disciplinary team and will consult with social workers, physiotherapists, dietician’s, Obstetricians, and diabetes educators, to ensure our clients are adequately supported during their pregnancy.
Whilst working in the Birth Suite, I see women presenting to be assessed for many different reasons such as bleeding, decreased fetal movements, abdominal pain, and we will care for women in labour. All women receive care from a midwife in labour regardless of their risk status, and care will be escalated for Obstetrician’s to review as needed.
We work very closely with our Obstetric team and have a great relationship as our goal is to ensure our clients receive the best care and have a good outcome. I also will work on our Women’s Ward, this is the ward that women are transferred to after having their baby. We support our clients with caring for their baby, assist with breastfeeding if needed, as well as monitoring for any complications post-birth.
Tell us about a piece of interesting equipment in your field of work.
We use Cardiotocography (CTG) machines, these machines allow us to continuously monitor the baby’s heart rate as well as to detect uterine contractions. We use these machines regularly in the hospital to check on fetal wellbeing and will use them in labour if indicated.
Your health service is seeing increasing complexity with 70% defined as high risk pregnancies. What is defined as a high risk vs low-risk pregnancy?
A low-risk pregnancy is one where the client has no Obstetric risk factors or other co-morbidities. Bearing in mind that the risk level can change if the client develops complications in pregnancy.
Whereas a high-risk pregnancy can be classified based on a large number of risk factors or co-morbidities. Some of these risks can include Diabetes (Type 1/Type 2/Gestational), Hypertension, Coagulation disorders, Cardiac issues, Heavy smoker, drug dependence. There are also Obstetric risks such as multiple pregnancies, small baby, history of postpartum haemorrhage, history of pre-eclampsia, or a BMI greater than 35. When risk factors are present we ensure that the client receives care from an Obstetrician and they may have more frequent appointments.
We are a large regional hospital so receive referrals from outlying areas, as these hospitals generally care for clients considered low risk, which means anyone that has a co-morbidity or risk factor may have to have their care in pregnancy (antenatal) and labour (intrapartum) transferred to our hospital. This is one of the reasons that we see so many high-risk clients.
What are some examples of the complications you experience / your midwives must clinically manage?
Postpartum haemorrhage (PPH) is when a client loses more than 500ml of blood after birth from the genital tract. A PPH is one of the major causes of maternal mortality in the world. Whilst we don’t have standing orders, all midwives should be skilled in managing a PPH. This involves recognising risk factors for PPH such as long labour, fast labour (under 4 hours), large baby, previous PPH, coagulation disorders etc.
We will give medications to try to stop the PPH, if the cause is due to trauma such as a tear, a midwife who is trained in suturing can repair the tear. This is an instance of midwives working closely with our medical colleagues to try and manage the PPH quickly and minimise blood loss.
There are other obstetric emergencies such as Shoulder dystocia, pre-eclampsia, HELLP syndrome, preterm labour, and it is not so much a change in our scope of practice but rather having the knowledge to manage each of these emergencies, as we are trying to ensure the safety of mother and baby.
Midwives will also closely monitor the baby’s heart rate in labour and will escalate care as needed if we have concerns.
What is antenatal care?
Antenatal care is caring for clients during their pregnancy. Continuity of care is seeing the same midwives throughout pregnancy and in labour. This has been proven to improve the rate of vaginal births. Whilst we provide continuity of care at our hospital, I do not work in that team. However, I do work in both Women’s Clinic where I provide antenatal care so at times I do see the same women in labour.
What are some challenges that Covid19 has given you and your colleagues/workplace?
Initially, Covid-19 was the great unknown, and we were not sure what the implications would be. As we work very closely with our clients, we very quickly had to increase our PPE and come up with procedures for caring for clients in labour with suspected or confirmed Covid-19. Covid-19 caused so much fatigue as there was a lot of wondering what was going to happen, and preparation needed, and staff cancelled annual leave to ensure we were all available.
Now we are seeing a large influx of clients and our birth numbers increasing this year as it seems many people decided to procreate in our various lockdowns. As with all of our colleagues in nursing and medicine, Covid-19 had such an impact on everyone’s mental health, and it was such a relief to be able to come to work and be surrounded by such a supportive team.
What advice do you have for junior midwives?
A willingness to learn, midwifery and obstetrics is not an exact science and it takes time and working closely with clients to develop the skills to recognise risks, and getting the skills to know when a client is in labour or when birth may be imminent. And even after developing that knowledge, we will always have clients that surprise us.
Being a student midwife is hard work, as there are many extra requirements such as a number of births you need to assist with and students need to follow a certain number of women through their pregnancy’s. It takes a lot of time but is definitely rewarding. Be patient, and remember that senior staff want you to succeed and no one knows everything. It is ok to admit if you need help or support.
To junior midwives, I would say that we never stop learning. Everyone can give you a different perspective, or a different way of performing a skill. I love working with so many people as I’m constantly seeing different ways to interact with people and your colleagues may have little tips and tricks to help you grow as a midwife. I would also say that it is ok to speak up if you are struggling, and it is important to ask for help. Our job can be overwhelming at times and there is no harm in seeking help or support, or debriefing when there is a difficult case. It is ok not to know everything.
What’s one of the greatest lessons you’ve learnt in your journey so far?
Listening is such an important skill, everyone has different experiences in their lives and they can teach us so much. I feel so lucky to have met and interacted with people from so many different walks of life, they have all taught me so much and made me appreciate what I have around me and they have helped me grow both professionally and personally.
What is one thing you wish you would have known before you started your career in this field?
It’s probably good that I didn’t know as I may not have taken this path if I did, but by starting this career I experienced so many challenges (the post-grad year is full-on), however, it is because of these experiences that I am the person that I am today. Where I work I am surrounded by people who are incredibly passionate and they have taught me so many things. As a result of their teachings, I have become a stronger person and I found a place where I feel at home.
Why should other nurses or students consider this area to work in?
Every aspect of nursing is a privilege as we are so fortunate to be able to provide care for people at every aspect of their lives. I love midwifery as I get to work closely with an amazing multi-disciplinary team and support people through pregnancy, labour, childbirth and after birth. It is such a special and momentous time and I feel lucky to be a part of it. Our job as midwives is much more than “catching or cuddling babies”.
What are the most challenging and difficult aspects of your area of work?
One of the things that I find challenging is the perception of some people that we want to intervene. At times I meet clients who feel that we are out to get them or are going to force treatment without getting consent. This is obviously not something that I am going to do but over time I have learned that this misconception can arise from fear or from misinformation on the internet. So to try and overcome this, I will talk to the clients and listen to their concerns. Listening is key because it helps me to learn why the client is concerned, and that way I can try and support them with their choices and let them know that I am here for them.
What is one myth or common misconceptions about midwifery?
Our job is not just about delivering babies or cuddling babies. We care for women who have lost babies either through miscarriage or stillbirth. We try our best to support them through their loss and try to find ways to remember their baby. We see and remember all of those baby’s that were lost, even if we don’t always talk about it.
What are some advice/thing’s others can do to better prepare themselves to get a job?
To be a midwife you either need to complete the double degree in nursing/Midwifery, complete a degree in midwifery, or if you are already a registered nurse – you can complete a 1-year postgrad diploma in midwifery. The model where you are employed whilst completing your postgrad can be quite competitive to get into, so don’t be afraid to show employers that you are passionate about midwifery when you get an interview.
Pre-Covid there were a number of companies that would conduct maternity focused study days aimed at nurses. If you are a graduate, ask if you could do an observation day to see if it is an area you may enjoy.
What pathway would you like to see the future of your profession take over the next 10 years?
I’d love to see more ability to offer women continuity of care, as we know this leads to improved outcomes. I’d love to see midwives better able to support Aboriginal and Torres Strait Islander women to birth on country and be supported by known midwives. Personally, I’d love to be involved in the work to improve maternal and neonatal mortality rates in countries like Papua New Guinea.
Who are the 3 people who have been most influential to you?
My dad is the reason why I wanted to be in healthcare, he is passionate about paramedicine, emergency management, and providing good care and he is always teaching me and challenging me to grow and evolve both personally and professionally.
My colleagues/family (both at work and St John) have supported me through so many things, they have helped me grow as a person, cheered me on to finish my postgrad after sustaining a broken ankle and helped me meet my requirements. They have hugged me, loved me and supported me through a divorce and they all continue to support me and help me juggle work and single parenting. I have become a stronger person because of their guidance and support (along with my family).
My daughter is amazing. She is 6 years old and is so strong, smart, sassy and independent. She inspires me every day and I always strive to be the person she deserves. Having her, helped me to see what was important to me and I feel so lucky to be her mum.
What areas of research are you interested in?
When women have babies, they can sustain tears, some of these tears (3rd and 4th-degree tears) can have lifelong consequences and some (not all) are preventable. I’ve been involved in a project to try and reduce the number of these tears occurring at our hospital. We did successfully significantly reduce this rate, however, it is work that is ongoing.
I have also been involved in a project to try and reduce the rate of stillbirth in Australia, this project involves providing education to clients on baby movements, sleeping position, and when to seek help from healthcare providers.
How can we work better with other health professionals in the multi-disciplinary environment?
Communication is key. At the end of the day we all want a positive outcome for our clients, so we should support each other to achieve this goal. There should not be an us vs them mentality. We need to work together and listen to each other.
Can you think of a really funny situation you’ve had while working?
Half funny – Half gross… Whilst caring for a woman in labour who was close to having a baby, her waters broke. Now despite me standing on the side of the bed, they managed to hit me straight in the face and avoided everybody else. Luckily my mouth was closed and I was wearing my PPE, so I helped that baby be born whilst amniotic fluid dripped down my face and hair. The doctor in the room very kindly wiped my face for me and once the baby arrived safely and the woman was comfortable, I left the room to shower and threw out my very soaked work shoes.
If you were invited to do a TED talk, what would be the title and what would you talk about?
Oh gosh, I don’t know… I want people to work better with our Aboriginal and Torres Strait Islander clients but it’s not something I’m an expert at either. I’ll just appreciate other people’s TED talks instead.
How do you destress after a shift and self-care?
Debriefing is important, I usually talk to my colleagues who are friends as at least they have an understanding of what my day has been like.
Night shift tips?
Be prepared!!! I bring in a healthy snack to eat at about midnight as I’m usually starving by then. I also bring in a smoothie in an insulated cup to drink at about 6 am so I can sleep well once I finish. I don’t nap but that’s just me as it makes me feel worse, everyone is different though.
Time management
Remember that we provide 24-hour care! I frequently see people stressing, working so hard to fit everything in their shift and sometimes staying back late. It is ok to hand over to the next shift. We need to change this culture.
Conflict resolution
It is so hard as we are all different. Taking a step back and walking away can be a good idea. Also trying to see things from the other person perspective helps. It is also ok to escalate things if you need to, so that management can support you to resolve conflicts.
What’s in your lunch box! What are some food tips/ideas for shifts?
I love a smoothie!!! It’s something I can drink on the go to work and is a great way to add in some extra nutrition. Insulated cups are amazing as they keep your smoothies cold and your coffee hot!!
For other midwifery related content go HERE
Check out Australian College of Midwives





You must be logged in to post a comment.