Table of Contents
We are fortunate enough to have Dr Jamie Durrant share his raw experiences on the Covid19 frontline.
Read on to find out how he went from an emergency nurse for 10 years in the NHS and Royal Navy to a dentist in general practice. And then from a Dentist to being a Senior Doctor (SHO) in a COVID19 assessment unit in 3 weeks!
An AUSMED Australia and The Nurse Break collaboration brings you this scrolling feed of stories from those on the frontline of the health service! Want to be featured here? GO HERE to learn more.
From nurse to dentist
My name is Jamie and a friend of mine working in Melbourne at the Alfred Hospital as a Registered Nurse asked me to write for The Nurse Break and share my experiences. We both worked together when I was a nurse in the Navy, we were both serving in Plymouth. So after a career in the Royal Navy and the NHS as a nurse, spending the majority of my time in Emergency Medicine, I decided a change was needed.
I’d spent just over 10 years in Emergency Care, and I needed a break. A career search identified that Dentistry was possibly a good match, I thought why not.
14 years on (9 Post-registration) I’m in general dental practice. My days were routine, almost simple; examinations, fillings, root cancels, cosmetic dentistry and injectables. Work and life were normal until there was a news report just after Christmas mentioning about this new virus, that has made the leap from ‘bats’ to humans and was causing havoc in a province in China.
The script from ‘Contagion’ and the NMC
I thought that’s like the script from ‘Contagion’ and that was the last I thought of it, and carried on with my daily life. Then it hit the UK, reports started coming in, the news started to report more and more cases. More importantly, close friends of mine that still work in emergency care, were dealing with it. The story’s soon started to filter through, the respiratory distress, the odd chest X-rays, staff members getting sick, and that it was spreading at an alarming rate. From my dental surgery, I was able to watch it unfold. Quickly I realised that as a dentist all we do is Aerosolized Generated Procedures (AGP’s) and this seemed to be part of the way it was spreading.
I had this ‘gut’ feeling life was going to change and that, my current role would be impacted. I spoke to the practice owner and the staff “oh your such a bringer of death Jamie’ was a comment I had made to me by one of the nurses, however, the principal dentist was just as concerned as me. For reference, this was about 7 weeks ago (written end of April 2020).
Quietly I made some enquiries. My initial reaction was to return to Emergency Nursing. After all, that’s where I was experienced in dealing with critically ill patients, despite the 8 years out of clinical practice! Things have moved on, or so I thought!!! Well, the Nursing and Midwifery Council NMC (UK) advised me when I contacted them that, my 10 years nursing expertise and all the time spent in Emergency Medicine, before my 9 years post reg experience as a dentist (we do a lot of emergency medical management as part of our CPD) “wasn’t applicable at this time”.
Ok, I thought, well I have friends that keep asking me to come back into acute care as we needed all hands on deck! Many people don’t realise the things general medicine dentists do. We are trained to take a history and to carry out system examinations. The news started to report possible lockdowns, that this ‘COVID 19’ was taking hold in the UK, I got this horrid sense of urgency that it was going to be bad. So again, reverting to type, I called the NMC.
There had been a report that the NMC and GMC were going to recall retired Nurses and Doctors to come and help. Great, that’s my call; again I was advised my skills were not applicable and I was out of date; we’ll surely anatomy hasn’t changed that much? Yes, I’d need a bit of training and some time to gain some experience but, better now while it is building than in the middle of the pandemic when so many people are sick?
Paramedic Ben
Then another friend of mine Ben called me. Ben had started as an operations manager in Emergency Medicine in an acute trust after 19 years as a front line paramedic. “Jambo, it is getting worse, the government have advised we start implementing a specific department to assess patients with symptoms…”
Other friends in NHS management positions were ‘warning’ me of what was coming, how bad it would get, there was even talk of a ‘Lockdown’ that may have to happen. Then Italy; I remember turning on the news and seeing patient after patient intubated and prone (I’d done a very small amount of ICU) – Proning a patient is, as many will know, one of the last things you can do, it is not great, it has massive issues, and patient after patient was prone in Italy… SHIT! This was my cue if that is happening in Italy, and all my friends were telling me about the pending crisis, then surely crisis planning that was being decided and that General Dentistry will stop; this was about 6 weeks ago.
I tried the NMC for the third time, yet I had received the same response. All I could hear was Ben in my head “you’re a bloody Dr, maybe you’re a dentist, but you’re a dentist who can prescribe and a dentist with an EM background, you’ll pick it up in no time”. So I called him, “Ben its Jambo, I need to do something to help, you and the rest of the people we know are telling me how bad is going to get and, well I don’t want to be sat at home knowing I can help’.
Yes typing that I know I sound like a total idiot but, that’s genuinely how I felt. One of the things I think you get from serving in the military is a sense of, we have to get this job done and someone has to do it. I needed to help ‘get it done’ to use one of the many phrases the Conservative Party kept using. Then the weekend of the 20th of March.
There had been little information given to the dental community. We were aware of the asymptomatic carriers, of AGP’s but… well things were moving so fast, writing this I can’t believe I’m talking about a matter of days and weeks.
So Friday the 20th at about 1630 we had our first guidance about reducing the amount of AGP’s we were producing, reduce the number of routine exams we were completing to prevent travelling and consider only completing emergency based dentistry. Saturday we had further guidance to limit treatments further, we spent the day writing policies to help the staff. Then on Sunday, the faculty released direct guidance that ALL AGP’s needed to stop, so in the space of 48 hours, Dentistry had stopped. I knew this was coming I called Ben and said what can I do. He said send me a CV and I’ll pass it around. Monday was spent in the practice calling patients, advising all the patients I’m treating with braces on how to manage them for the future time.
How long? Was the question all of them asked, all I could say was ‘I don’t know’. We closed the practice. Tuesday my first day working from home. I spent it calling people trying to find a way into secondary care. The reports were coming in thick and fast how quickly it was spreading. Life was racing by at 200mph. Dealing with patients, helping close down the practice, discussing with my mum about getting her down as I’d need help with my children, worrying about how I would pay my rent as I’m self-employed.
Dentist becomes Medical Doctor
Then the lockdown happened. Ben came through.
He had managed to get me an appointment with the Medical Director at the trust he works in. I was met by an incredibly stressed medical director, the interview was literally ‘do you want to come back as a nurse or as part of the medical team?’. Well, I can’t come back as a nurse as I’m not registered with the NMC was my response. ‘OK so as an SHO then?’. And that was it, 20 mins later Ben called me to say ‘can you go to gastro their SHO is self-isolating’ and that was it, suddenly I’m an SHO in the medical team of a lovely 306-bed acute trust. All the staff from the consultants to the cleaners have been so supportive and have taken me under their wing. The learning curve over the past 3 weeks has been astronomical. I can’t believe it is only been 3 weeks!
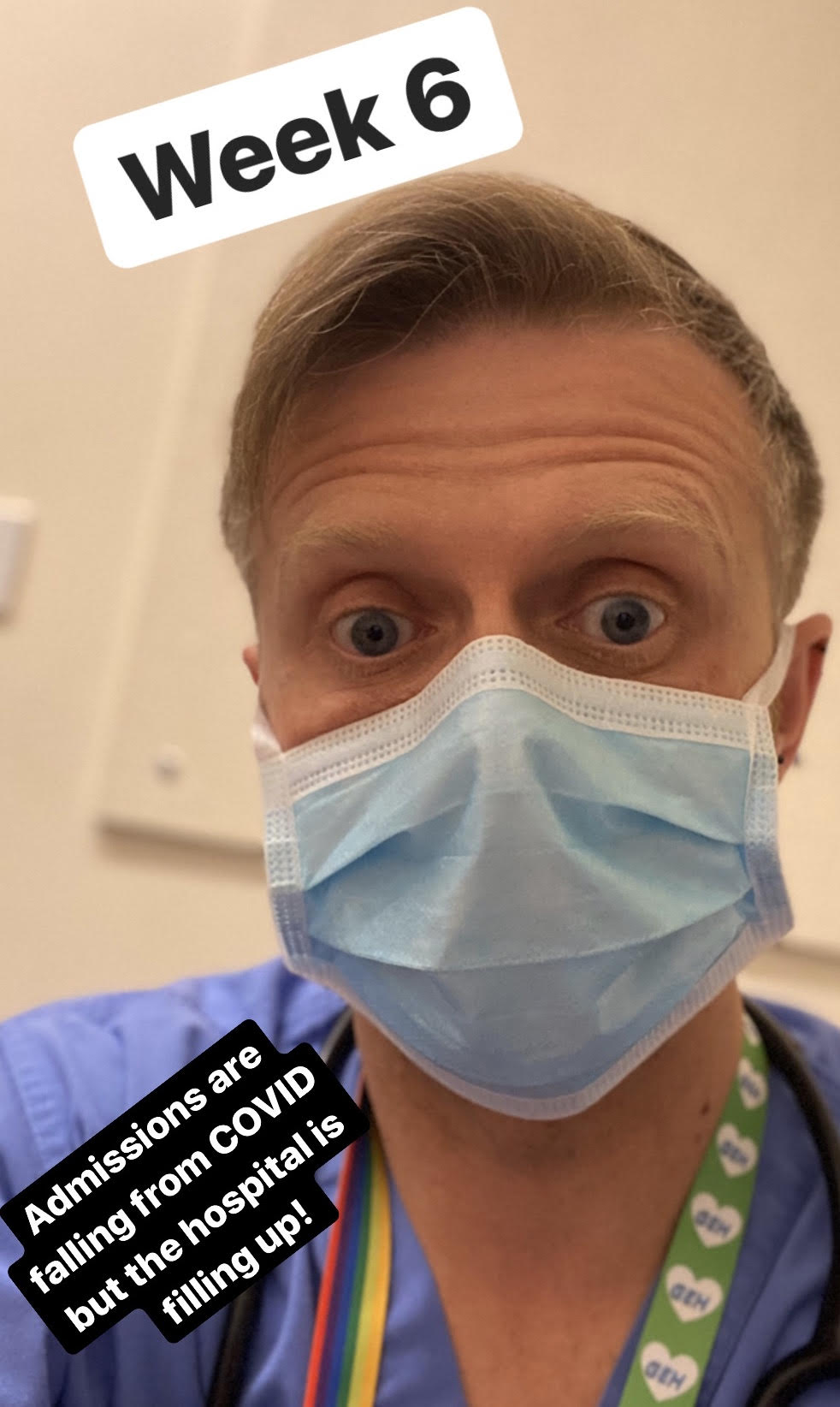
So this is what I’m doing; I’ve gone from a dentist in general practice to being an SHO in ‘ED2’ which is a COVID 19 assessment unit.
This is the end of my 3rd week. The first week I spent on days. Gastro, CCU and Medical Assessment. The medical director wanted to give me a bit of an introduction before ‘it started’. Then it was on to nights! Last week I did 4 nights. The first set of nights in 9 years!!! And it killed me. We were steady, constant but steady. This week I was on nights again (I filled in last week but my ‘line’ on the rota was nights again), and god this week was busy.
The press release from the government today said it was plateauing, that admissions were getting less, well they didn’t tell the patients that here. I’ve gone from assessing peoples teeth too listening to chests, interpreting chest x-rays, being involved in completing ‘respect’ forms on patients to ensure their ceiling of care is appropriate (as in should they go to ICU?) and, prescribing drugs that I need to check the spellings of! I’m so out of my comfort zone I can’t tell you.
But I’m safe, the teams are supportive and the education I’ve received has assisted me to transition smoothly into my new role. I’ve almost forgotten how to complete a root canal! The Chief Dental Officer in a recent webinar said that dentists are ‘head and neck specialists’ and she is right we are, that as a profession we need to broaden the boundaries and, well, I’m doing that.
It’s indiscriminate of who is well and who decompensates
Patients are so sick! That’s the shocking part of it. And it’s indiscriminate of who is well and who decompensates. When they become sick it happens quickly. Yes, this is a respiratory based virus but, the number of patients that have other symptoms is mind-blowing. As a team, we have dealt with 3 serious cases of a septic shock this week, and that isn’t including the patients that have gone into ARDS! My first week on nights, the House officer on-call for the wards asked me to accompany her to a sick patient.
He was a 49-year-old, fit and well builder. He had been admitted 48 hours earlier and, well he was deteriorating. We arrived on the ward and I was presented with one of the sickest patients I’ve seen in all of my 23 years in healthcare. He was grey, cyanotic to the point it looked fake! Like those actors, we get to use on the OCSE examinations!! But this wasn’t a simulation this was real, from somewhere in the back of my brain the years of ED nursing, ALS training, medical emergency training and my medical training just seemed to click.
There were about 30 seconds of panic;
It felt like a lifetime, and then suddenly the HO asked ‘shall I bleep ICU outreach?’. I remember replying ‘yes’ and then suddenly all those years of training kicked in.
A) he has one
B) his respiratory rate is too fast (44), his O2 saturation’s were through the floor (75%) on 100% O2, I listened and there was so little air movement. ‘Shell I get the blood gas?’ She was back from bleeping outreach ‘yes please’, said secretly I was thinking ‘thank god’ – yes I can take gasses I’d been doing them all night but for some reason. I froze and noted more I can do on B), until the gas was back, ‘Hang on’ I remember saying, ‘call X-ray I need a portable chest urgently’.
C) access he has; he has a Blood pressure above 100, a pulse of 140 per min but, that’s compensating from his respiratory distress.
D) he was conscious, able to talk in gasped words, ‘can you call the reg when you have the gas’ I said to the HO. ‘I can’t he is in resus with an arrest’ was the reply. ‘So it is just me’ I thought.
I’ve been re-reading I’ve had re-training and suddenly, ‘the dentist’ is leading this team. I known what he needs before the gas comes back, he needs CPAP possibly even intubating. But, we are trying to put that off as long as possible in the UK as the mortality correlation with ventilated patients is huge (at our trust we only extubated our first patient today, they have been managing this here for weeks!).
The gas comes back, in the hands of the outreach nurse, she arrived with an angel-like glow around her (Or at least that’s how it felt!). She hands me the gas and says ‘I think CPAP, you?’. And I look at the results and I know what they mean and, well that’s it I’m suddenly ‘the Dr’.
The decision was made ‘Yes, start him on a PEEP of 12 at 60% O2’. 2 hours later he is talking to me, thanking me for helping him. All I want to do is fall into a snotty heap on the floor but, I can’t, I’m a professional and, this is what is needed. Did I ever feel he was not in safe hands, NO!
Did I ever feel like I was flying by the seat of my pants as this is so pushing my boundaries; every agonisingly long second. But ‘on reflection’ all that knowledge and training and experience did their job, sorry NMC your wrong my skills are needed. You ask James!
He spent 5 days on CPAP, had some rough times in that time, was proned on CPAP as still, his lungs struggled but, I went to see him today and he is off the CPAP and on very little oxygen support. I have treated other patients since him and will treat more, but James was my first and I will always remember that episode. It is hard, I feel out of my depth at times and am so glad I’ve got the support of some amazing nurses and incredible medical colleagues.
Support and teamwork saving lives
If I ever felt I was putting people at risk I’d be out of here, but I’m not. The more shifts I do, the more I learn the more my medical knowledge increases, the less of a fake Dr I feel. I go onto days next week. I’m starting as the SHO on CCU so, as well as seeing my children for the first time in 3 weeks (My youngest had symptoms so my ex and my children were self-isolating for 2 weeks), I need to do some serious revision on the heart and those wriggly lines they call an ECG!! But, again I know I’ll be supported. All I keep getting from the consultants and senior registrars is ‘thank you for stepping up and helping, it’s appreciated’.
All I feel is that I’m having to be supported by them, its an odd paradox. But I’m here, I’m helping, I’m making a difference to the patients and, well, regardless of the speciality we are health care professionals and, that’s what we came into healthcare for! The UK government announced today a further minimum lockdown of 3 weeks, so I’ll be here for some time yet!
Stay Home, Save lives, protect our NHS. (if you’re not reading this in the UK, please from a Dentist working in acute medicine… Stay home! Flatten your curve! Stop the spread!).
Dr Jamie Durrant
Fellows BDS BSc(Hons)
Clinical Lead Periodontics and Facial Aesthetics
Associate Dentist VIDA Dentistry Fareham
Aesthetic Medicine Practitioner
Lead Trainer KT Training








I like the helpful info you provide in your articles. I will bookmark your blog and check again here regularly. I’m quite certain I’ll learn a lot of new stuff right here! Best of luck for the next!
Primary Care Physicians New Braunfels