Table of Contents
Journey from Australian hospitals to the Solomon Islands as Frances Kennedy shares her experiences volunteer nursing. Learn about the challenges, the rewards, and the power of laughter. Dive into this captivating story and explore more articles, engage with vibrant Nurses Collective groups, and share your own adventures – email us today at hello@thenursebreak.org
Introduction
Welkam, iu olgeta from the Solomon Islands! Writing this I’m looking through the coconut palms at the ocean, a cool breeze is blowing and a gaggle of kids are leaping off rocks into the surf. Idyllic, no? Well, mostly…
22 years of nursing
Next month will see my 22nd anniversary as an RN – where does the time go? Seems like yesterday when I started at the Royal Brisbane Hospital, chuffed in my starched uniform and shined shoes and sure people were looking at me, thinking, “Wow, a nurse!”. From then I worked in emergency and ICU nursing, mostly in major hospitals, learning how to manage critically-ill patients with myriad complex equipment, supported by well-resourced, experienced teams – none of which prepared me whatsoever for nursing in the Pacific!
Papua New Guinea Volunteer Nursing
In 2016, perhaps a little burnt-out from demanding EDs, I moved to Papua New Guinea with my husband who was already working there and landed a job with a company to manage eighteen clinics across the country, staffed solely by nurses. The public health system in PNG, as in many of the Pacific nations, is extremely stretched and poorly-resourced, and people often resort to privately-run clinics – in some of ours, the two nurses saw up to 100 patients a day. Steep, steep learning curve but I loved seeing patients, working with and advocating for nurses (pay-rises all round!) and travelling the country. It’s impossible not to fall madly in love with the beauty of PNG and marvellousness of her people but I definitely won’t miss the toe-curling flights that dodge through the mist-clouded mountains into the Highlands.
Australian Volunteers International –
In 2018 we moved to Honiara and I was accepted by Australian Volunteers International as an ED nurse advisor based at the National Referral Hospital, fortunately landing in a program that had previously been supported by two highly-experienced nurse volunteers and ACEM, as well as a great team of local clinicians. By then I’d learned a little of Pacific ways and somewhat prepared for lesser-resourced settings but, woe, my proudly-cultivated PNG Pidgin wasn’t much use and had to start again with the Solomon Islands version (btw, your bladder and uterus is ‘basket blong mimi’ and ‘basket blong pikinnini’ – isn’t that heaven?).
As well as spending quite a bit of time in direct patient care, I worked with the ED nurse educator to implement programs to support education and quality-improvement: sepsis management, recognition and management of the deteriorating patient, ALS and APLS, protocol development, competency-based assessments, patient flow and trauma. We also travelled to one of the provinces (another fun-filled flight in a storm) to provide teaching to doctors and nurses who don’t have regular access to educational activities.

ED Sepsis Awareness Launch

Travelling to Malaita with ED doctors
The Solomon Islands University does not have a medical faculty and so their doctors study in other countries – Cuba, China, Fiji, PNG and Taiwan – and sometimes struggle a little on their return. AVI had implemented a valuable program to support these ‘bridging interns’ but unfortunately all volunteers were repatriated with the advent of COVID-19, leaving the sustainability of the program in jeopardy. I chose to remain in-country (I have dogs! Oh, and a husband, who admittedly comes a distant second) and AVI’s flexibility and commitment allowed me to continue, also taking on the role of coordinating the bridging program by ensuring a regular teaching and assessment schedule. It was a little overwhelming at first and my experience with medical education was exactly zero but the volunteers supported remotely, DFAT provided assistance and the local consultants rose brilliantly to the occasion – I’m very proud to report those terrified little interns had a 100% pass rate and blossomed into more competent, confident clinicians.
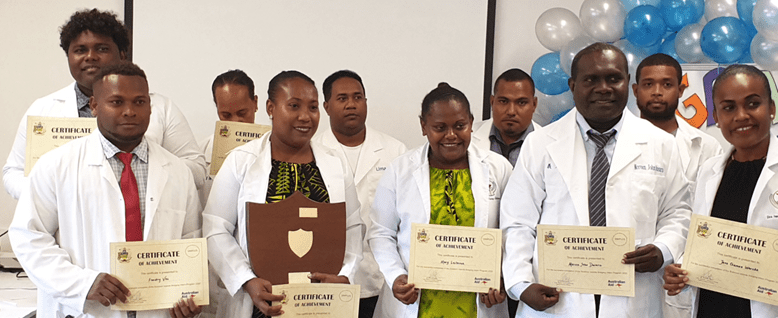
Bridging interns graduating
A new role
Since last year I’ve moved on from AVI into an Infection and Prevention Control advisor role supported by DFAT. Again, a steep learning curve, the challenges are significant: overcrowding, prolonged lengths-of-stays, ageing infrastructure, a lack of antibiotics and lab diagnostics and a moodily temperamental incinerator but we’ve developed a great team of physicians, pharmacists, microbiologists and nurses and implemented some programs – audits, teaching, reporting, a hospital-wide AMS committee and weekly clinical reviews- that are becoming embedded and showing improvements. Perhaps my favourite memory was when I MRO-swabbed nearly every patient in the hospital and my mum who was visiting came to help by completing the path requests. My mum was a NICU midwife and, NO offence to you NICU nurses out there but you often are quite “bare-below the armpits, quadruple-check everything, 0.001 mls” nurses. My poor mother would ask me the patient’s date-of-birth and, as many Solomon Islanders don’t know their DOB, I’d glance over and reply, “About 45?”. And when some of them casually waved away the privacy screen and pulled down their shorts in full view of the ward, I thought she was about to have a seizure. The patients and I ended up falling on top of each other, hysterically laughing at her horror. She still talks about that time with a slightly wild look in her eyes.
Finally, a 14-bed HDU, built and equipped by DFAT, is now operational. It has been a huge undertaking, over a year in development and difficult in the beginning as the project managers were all in Australia so we had to conduct all planning via Zoom. I used to come home to my husband, a builder, and ask what’s an architrave? As well, the medical nurses had little experience with rhythm interpretation, blood gas analysis and advanced assessments which required an extensive training program but we now have a beautiful, clean, well-equipped area to manage our sicker patients by more confident nurses who are proud of their HDU.
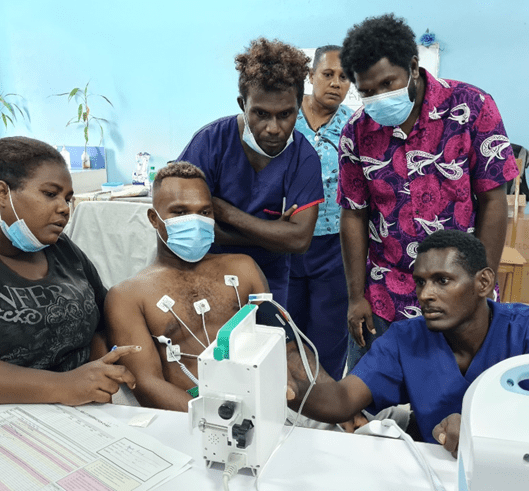

HDU nurses in training
Challenges and Rewards
- Working in a different healthcare system and culture can be challenging. What are some of the unique challenges you’ve faced as a nurse in the Solomon Islands, and how have you addressed them?
- On the flip side, what have been the most rewarding aspects of your work in the Solomon Islands, both professionally and personally?
The constant lack of resources can be quite difficult to manage with the most basic of items – paracetamol, gauze, various antibiotics, thermometers, KY, ECG dots – often unavailable. Seriously, I dream about Primapores! You realise how spoilt we are in a country like Australia where most things are at your fingertips. I shudder when I think how much we waste: “Oh, it’s a double-lumen central line. I need a triple so oops, let’s just toss this one…”. It does make you quite resourceful though. Who would’ve thought IDCs make wonderful door-closers and that peanut butter mixed with coconut milk helps when you don’t have NGT feeds?
Jokes aside, I did initially find it challenging and sometimes distressing when there were poor outcomes associated with a lack of resources. It still does, at times. But I try to remember that we all do our best with what we have and having fancy, higher-cost therapies only benefits a few. And I’ve become a brilliant scrounger – it’s amazing what you can inveigle out of visiting medical teams or even poor, unsuspecting visitors who bemusedly find themselves carrying in blood culture bottles in their carry-on!
What makes it worthwhile? Far, far, far away, the patients and my colleagues. Solomon Islanders are the most forgiving, brave, merry, dignified people and, even after five years, I still find myself in awe of their strength in adversity and appreciation for anything you try to help with. And the doctors and nurses…the conditions they work in, their commitment and versatility – I have no words. Oh, and that there’s no Falls risk or Riskman or endless paperwork

Pretty good sanitary pads can be made out of cotton wool and gauze!
Future Endeavors and Advice
- Could you share your insights on the importance of nurse-related roles in the Solomon Islands and other similar settings?
- Finally, what advice / resources would you give to healthcare professionals who are considering volunteer work in underserved regions like the Solomon Islands? What personal qualities and skills are particularly valuable in such roles?
Nursing roles in the Solomon Islands are sometimes neglected compared to medical roles. Doctors tend to get more funding and scholarships for overseas study and experience, both of which are invaluable for growth of expertise and exposure to new practices. Nurses here have roles such as CNs and CNCs but they don’t really know what that means as they’ve never seen it or had it modelled. As well, many of them are women and are also responsible for childcare, housework, shopping etc so that limits their opportunities even further.
These issues not only complicates nursing growth but also impacts directly on the health of Solomon Islanders as nurses often are responsible for primary health care, particularly in the provinces where the Area Health Centres are managed without medical input.
That said, our nurses have amazing skills and really are Jacks-of-all-trades. Cannulate a premmie, deliver a baby, suture up a huge lac, set a fracture? Easy peasy!
My suggestions if you’re considering volunteering here?
1. Learn the language. No-one cares if you’re hopeless at it, just that you have a go.
2. Ease into it. There is usually a reason for everything but it’s not always apparent at first.
3. Bake a cake occasionally. All nurses like cake.
4. Don’t eat skyfruit. They’ll tell you it’s good but it is truly, truly dreadful.
5. They’ll try to dress you up and make you sing with them. Let them.
6. Have a laugh with them. Once they accept you, you’ll all be laughing your heads off.
7. Be prepared to have a go at something new or out-of-the-box. Challenges help you grow, both personally and professionally.
8. Remember, you’ll learn more from them than they’ll learn from you. I promise you’ll be a better practitioner for it.






You must be logged in to post a comment.